Research Article - Clinical Schizophrenia & Related Psychoses ( 2022) Volume 0, Issue 0
The Insulin and Glycemic Parameters Role in the Sleep and Depression Disorders in Diabetes Mellitus Type 2 Patients
Waleed Azeez AlAmeedy1, Taha H. Alnasrawi2, Zainab A. Mahdi3, Tawfeeq Alghazali4, Ahlam Kadhim Hussein5, Muneam Hussein Ali6, Hajer Ali Enad7, Karrar A. Zwain8* and Ali Jali Obaid92Department of Nursing, University of Warith Al-Anbiyaa, Karbala, Iraq
3Department of Nursing, University of Kerbala, Kerbala, Iraq
4Department of Journalism, The Islamic University in Najaf, Najaf, Iraq
5Department of Nursing, Al-Zahrawi University College, Karbala, Iraq
6Department of Nursing, Al-Nisour University College, Baghdad, Iraq
7Department of Medical Laboratory Techniques, Al-Mustaqbal University College, Babil, Iraq
8Department of Nursing, Altoosi University College, Najaf, Iraq
9Department of Medical Laboratory Techniques, Hilla University College, Babylon, Iraq
Karrar A. Zwain, Department of Nursing, Altoosi University College, Najaf, Iraq, Email: karrar.zwain@altoosi.edu.iq
Received: 05-May-2022, Manuscript No. CSRP-22-62837; Editor assigned: 09-May-2022, Pre QC No. CSRP-22-62837 (PQ); Reviewed: 23-May-2022, QC No. CSRP-22-62837; Revised: 30-May-2022, Manuscript No. CSRP-22-62837 (R); Published: 07-Jun-2022, DOI: 10.3371/CSRP.AWTH.060722
Abstract
The role of insulin and glycemic parameters have been well described in diabetes mellitus and its complications, in this study the relation of sleep disorder with insulin and glycemic parameters were detected in Diabetes Mellitus Patients Type 2(DM2) and DM2 suffered from Depression Disorder (DD), the glycemic parameters including (Fasting Blood Glucose (FBG), glycated protein (HbA1c), Insulin Resistance (IR) and Insulin Sensitivity (IS) and Insulin Level (IN) were detected. Results show that sleep duration in DM2 and DM2 with DD were in non-significant differences among groups, the DM group having less than 6 hours of sleep was lower percentage than DM2 with DD and control groups. significant changes in all glycemic parameters and insulin level were observed among groups, non-significant changes of all study variables between>6 hours and<6 hours subgroups excepted the FBG in the control group that has significant changes (p=0.009), the correlation of sleep duration with IN and glycemic parameters show non-significant changes in DM2, DM2 with DD in comparison with the control group, there was weak positive correlation between sleep and FBG, IR in DM2 with DD and weak inverse with DM2, positive correlation with IS in DM2, and strong association with IN in DM2 with DM and inverse correlation in DM2. The study concluded that glycemic parameters didn’t associate with sleep duration, but insulin may contribute to the sleep duration in DM and DM2 with DD according to its correlation in study groups.
Keywords
Insulin • Glycemic parameters • Sleep disorder • Diabetes mellitus type 2 • Depression disorder
Introduction
Diabetes mellitus is the common health problem impact on the quality of the person life by increasing complication and mortality, sleep disorder is less known factor for DM2 development, a sleep disorder effects on quality, duration lead to detrimental impacts on metabolism of glucose and weight regulation. An Investigation has sleep duration<5 h, insomnia and Obstructive Sleep Apnoea (OSA) and poor quality are correlated with the DM2 development [1,2]. The sleep disorder association with DM has been found a probably higher than in the general population, it's also caused faster progression of DM and play an important role in DM management [3].
From one of the most co-morbidities with DM is a depression [4,5]. The DM patients, those suffered from depression have more DM complications than others that lead to huge dysfunction and bad life quality [6-11] in comparison with normal mood state. Studies found Poor sleep quality was significant in predicting diabetes-related quality of life after controlling for age, duration, type of complications, insulin level, depressive symptoms, physical activity [12,13]. The current study aims to detect the association between insulin, glycemic parameters and sleep disorder in diabetes mellitus type 2 patients with and without depression disorder.
Materials and Methods
The present study included diabetes mellitus type 2 patients, diabetes mellitus type 2 with depression, and depression patients and healthy individuals as a control group. All patients were male, Blood samples were collected from each contributor, according to ethical approval of the ministry of environment and health, insulin and glycemic parameters including (FBG, HbA1c, IR and IS) by classical laboratory methods, the age range of DM2 with DD (22 years to 67 years), DM2 (20 years to 56 years) and control group was (19 years to 53years). The depressed patients were diagnosed by specialist psychiatry prof. Dr. Arafat Al-Dujaily in college of medicine/ Kufa University. Data were represented as mean ± SE, ANOVA one way; independent t test and correlation were used to statically analysis of data at p less than 0.05.
Results
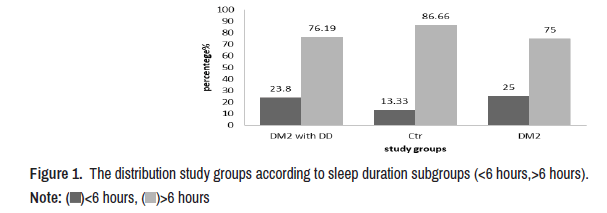
In the present study significant differences in FBG, HbA1c, IN, IR and IS (p=0.000) and non-significant in sleep duration (p=0.343) (Table 1). The study groups were distributed according to sleep duration into two subgroups<6 hours and>6 hours, high percentages observed in all groups that have>6 hours than sub-group<6 hours. The subgroup<6 hours in the DM2 with DD was (23.8%) and in DM2 group (25%), while in the control group was (13.33%) (Figure 1).
| Study group | FBG mg/dl | HbA1c% | IN µIU/ml | IR | IS | Sleep (hours) |
|---|---|---|---|---|---|---|
| DM2 with DD | 279.33 ± 27.73 | 9.79 ± 0.50 | 1.32 ± 0.21 | 0.92 ± 0.20 | 0.41 ± 0.01 | 7.33 ± 0.42 |
| DM2 | 222.66 ± 18.1 | 8.56 ± 0.29 | 4.09 ± 0.45 | 1.90 ± 0.22 | 0.37 ± 0.01 | 8.05 ± 0.38 |
| Ctr | 94.36 ± 2.57 | 5.14 ± 0.06 | 2.56 ± 0.181 | 0.59 ± 0.045 | 0.42 ± 0.008 | 8.10 ± 0.25 |
| P value | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.343 |
The insulin level and glycemic parameters in study groups according to sleep duration, the results show significant changes in the control group in FBG. Non-significant changes observed in IN level and glycemic parameters. IN increased in DM2 with the DD group in>hours. While other changes were slightly (Table 2). The correlations between sleep duration with insulin and glycemic parameters shows that the FBG weak positive correlation with sleep duration in DM2 with DD while inverse correlate in control group and DM2. The HbA1c inverse correlated with sleep duration in all study groups. Insulin shows positive correlation with sleep duration in the control and DM2 with DD groups and inverse in DM2 group. IR was an inverse correlated with sleep duration in control and DM2 groups and positive correlated in DM2 with DD. Finally IS inverse related with sleep duration in the control group and DM2 with DD and positive correlated in DM2, notably all correlations were non-significant differences (Table 3).
| Glycemic parameters | <6 hours | >6 hours | sig |
|---|---|---|---|
| FBG mg/dl | |||
| DM2 | 220.60 ± 36.33 | 219.23 ± 21.00 | 0.974 |
| DM2 with DD | 275.80 ± 23.72 | 280.43 ±36.03 | 0.945 |
| Ctr | 111.00 ± 4.60 | 91.80 ± 2.55 | 0.009* |
| HbA1c | |||
| DM2 | 8.60 ± 0.63 | 8.43 ± 0.33 | 0.802 |
| DM2 with DD | 11.18 ± 1.14 | 9.36 ± 0.53 | 0.131 |
| Ctr | 5.35 ± 0.15546 | 5.1138 ± 0.071 | 0.232 |
| IN µIU/ml | |||
| DM2 | 4.12 ± 0.924 | 4.02 ± 0.51 | 0.923 |
| DM2 with DD | 0.74 ± 0.168 | 1.50 ± 0.26 | 0.131 |
| Ctr | 2.55 ± 0.53 | 2.56 ± 0.197 | 0.989 |
| IR | |||
| DM2 | 1.87 ± 0.41 | 1.86 ± 0.26 | 0.989 |
| DM2 with DD | 0.52 ± 0.170 | 1.05 ± 0.25 | 0.281 |
| Ctr | 0.70 ± 0.16 | 0.57 ± 0.046 | 0.316 |
| IS | |||
| DM2 | 0.37 ± 0.02 | 0.37 ± 0.011 | 0.880 |
| DM2 with DD | 0.42 ± 0.015 | 0.41 ± 0.016 | 0.769 |
| Ctr | 0.41 ± 0.02 | 0.42 ± 0.008 | 0.676 |
Note: *: Statistically significant at p ≤ 0.05. |
|||
| Correlation | FBG | HBA1c | IN | IR | IS | |
|---|---|---|---|---|---|---|
| Ctr | r | -0.240- | -0.085- | 0.080 | -0.002- | -0.047- |
| p | 0.201 | 0.654 | 0.674 | 0.992 | 0.805 | |
| DM2 with DD | r | 0.157 | -0.256- | 0.409 | 0.181 | -0.037- |
| p | 0.495 | 0.262 | 0.066 | 0.432 | 0.873 | |
| DM2 | P | -0.015 | -0.164 | -0.277 | -0.324 | 0.249 |
| r | 0.926 | 0.318 | 0.088 | 0.044 | 0.127 | |
Discussion
The current results indicate that there were low percentage of study groups have<6 hours than>6 hours, and sleep duration slightly affected by insulin and glycemic parameters. The studies of epidemiologic and clinical data concluded that Obstructive Sleep Apnea (OSA) contributed to the changes in the glucose metabolism pathogenesis which increased developing DM2 resulting from short sleep duration, also sleep disturbances associated with DM2 even with absence of complications or obesity [14,15]. The disorder in sleep cusses insulin resistance and dysfunction in beta cells by some pathways [16], these pathways included Hypoxia, fragmentations of sleep, and sympathetic nervous system activation [17-23]. The Sleep fragmentation leads to increase in the activity of sympathetic, elevation of inflammation level, obesity and adipose tissue inflammation [24,25]. Kent, et al. found that Intermittent Hypoxia (IH) and sleep deprivation likely have major role in the glucose metabolic dysfunction pathogenesis in OSA, thus involved in the different pathways synergistic with obesity [26], all thought of slightly effect of sleep duration in the glycemic parameters in the current study, the epidemiological and experimental evidences observed that OSA results in glucose intolerance, that cusses T2DM [27-30].The disturbance in sleep has also impacted in the some physiological alteration like cortisol and ghrelin elevation, leptin levels decrement, and impaired glucose metabolism [31].
The weak correlation of sleep duration and glycemic parameters in study groups didn’t agree with other studies, this may be the lifestyle of the Iraqi population in nutrition, physical activities, type of medications and mood state, furthermore the co-morbidity with depression also may be effected, moreover, glucose, protein and lipid turnover displays an important variability through the natural sleep/wake cycle that is independent of alteration of metabolic stimulate by food intake. For instance the glucose level of plasma strongly follows the circadian pattern and progressively raised during sleep with the highest levels in the early morning [32-34]. Diurnal differences in metabolism of glucose are mediated primarily during direct autonomic innervation of target organs from the SCN [35], and are independent of circulating glucagon or insulin levels [36,37]. In fact, the output of suprachiasmatic nucleus-driven autonomic was shown to control the hepatic glucose output [35,38,39], and is most likely also contributed in the skeletal muscle blood flow lowered and muscle glucose uptake decrement during sleep [38-40].
There were other factors may be involved in the sleep duration like neurotransmitter levels in study groups especially in depression patients that suffered from unstable level of these neurotransmitter such as melatonin, serotonin and dopamine that have a crucial role in sleep quality and duration [41]. The length of time that insomnia lasts and how frequently it happens vary. One in ten persons who suffer from chronic insomnia and almost half of all adults who do have occasional attacks of sleeplessness. Insomnia can develop on its own or be linked to physical or mental health issues. Short-term (acute or adjustment insomnia) or persistent insomnia are also possible (chronic insomnia). Additionally, it may come and go, with intervals when a person experiences no sleep issues. Chronic or adjusting insomnia might persist for a few weeks or only one night. When person experiences insomnia at least three nights per week for a month or more, their insomnia is considered chronic. Stress in life (such as job loss or change, death of a loved one, or moving), illness, or environmental variables like light, noise, or severe temperatures can all contribute to short-term or acute insomnia.
Long-term or chronic insomnia (defined as insomnia that lasts for three months or longer and happens at least three nights a week) can be brought on by conditions like depression, ongoing stress, and night time pain or discomfort. A conditioned emotional response is a frequent contributor to chronic sleeplessness. Insomnia symptoms are sometimes prolonged by thoughts about the sleep issue (such as "What if I don't fall asleep tonight?") and behaviours that emerge in response to the issue (such as sleeping in and taking naps, daydreaming in bed).
Conclusion
The impact of sleep disturbance in the insulin and glycemic parameters in DM2 and DM2 with DD were investigated in current study, output concluded, Results show that sleep duration in DM2 and DM2 with DD were in non-significant differences among groups, the DM group having less than 6 hours of sleep was lower percentage than DM2 with DD and control groups, the study concluded that glycemic parameters didn’t associate with sleep duration, but insulin may contribute to the sleep duration in DM and DM2 with DD according to its correlation in study groups.
References
- Anothaisintawee, Thunyarat, Sirimon Reutrakul, Eve van Cauter and Ammarin Thakkinstian. "Sleep Disturbances Compared to Traditional Risk Factors for Diabetes Development: Systematic Review and Meta-analysis." Sleep Med Rev 30 (2016): 11-24.
[Crossref] [Google scholar] [Pubmed]
- Yuan, Shuai and Susanna C. Larsson. "An Atlas on Risk Factors for Type 2 Diabetes: A Wide-angled Mendelian Randomisation Study." Diabetologia 63 (2020): 2359-71.
[Crossref] [Google scholar] [Pubmed]
- Schipper, Samantha BJ, Maaike M. van Veen, Petra JM Elders and Annemieke van Straten, et al. "Sleep Disorders in People with Type 2 Diabetes and Associated Health Outcomes: A Review of the Literature." Diabetologia 64 (2021): 2367-77.
[Crossref] [Google scholar] [Pubmed]
- Katon, Wayne, Elizabeth HB Lin and Kurt Kroenke. "The Association of Depression and Anxiety with Medical Symptom Burden in Patients with Chronic Medical Illness." Gen Hosp Psychiatry 29 (2007): 147-55.
[Crossref] [Google scholar] [Pubmed]
- Alonso-Morán, Edurne, Altynai Satylganova, Juan F. Orueta and Roberto Nuño-Solinis. "Prevalence of Depression in Adults with Type 2 Diabetes in the Basque Country: Relationship with Glycaemic Control and Health Care Costs." BMC Public Health 14 (2014): 1-8.
[Crossref] [Google scholar] [Pubmed]
- Öztürk, Zeynel Abidin, Yusuf Yesil, Mehmet Emin Kuyumcu and Esen Savas, et al. "Association of Depression and Sleep Quality with Complications of Type 2 Diabetes in Geriatric Patients." Aging Clin Exp Res 27 (2015): 533-8.
[Crossref] [Google scholar] [Pubmed]
- Egede, Leonard E. "Diabetes, Major Depression, and Functional Disability among US Adults." Diabetes Care 27 (2004): 421-8.
[Crossref] [Google scholar] [Pubmed]
- Kohen, D., A. P. Burgess, J. Catalan and A. Lant. "The Role of Anxiety and Depression in Quality of Life and Symptom Reporting in People with Diabetes Mellitus." Qual Life Res 7 (1998): 197-204.
[Crossref] [Google scholar] [Pubmed]
- Ali, Saima, Margaret Stone, Timothy Chas Skinner and Noelle Robertson, et al. "The Association between Depression and Healthâ?Related Quality of Life in People with Type 2 Diabetes: A Systematic Literature Review." Diabetes Metab Res Rev 26 (2010): 75-89.
[Crossref] [Google scholar] [Pubmed]
- Chyun, Deborah A., Gail D. Melkus, Deborah M. Katten and Wendie J. Price, et al. "The Association of Psychological Factors, Physical Activity, Neuropathy, and Quality of Life in Type 2 Diabetes." Biol Res Nurs 7 (2006): 279-88.
[Crossref] [Google scholar] [Pubmed]
- Verma, Swapna K., Nan Luo, Mythily Subramaniam and Chee Fang Sum, et al. "Impact of Depression on Health Related Quality of Life in Patients with Diabetes." Ann Acad Med Singap 39 (2010): 913-7. [Crossref]
[Google scholar] [Pubmed]
- Luyster, Faith S. and Jacqueline Dunbar-Jacob. "Sleep Quality and Quality of Life in Adults with Type 2 Diabetes." Diabetes Educ 37 (2011): 347-55.
[Crossref] [Google scholar] [Pubmed]
- Wändell, Per E. and Jonas Tovi. "The Quality of Life of Elderly Diabetic Patients." J Diabetes Complications 14 (2000): 25-30.
[Crossref] [Google scholar] [Pubmed]
- Zizi, Ferdinand, Girardin Jean-Louis, Clinton D. Brown and Gbenga Ogedegbe, et al. "Sleep Duration and the Risk of Diabetes Mellitus: Epidemiologic Evidence and Pathophysiologic Insights." Curr Diab Rep 10 (2010): 43-47.
[Crossref] [Google scholar] [Pubmed]
- Trento, Marina, Fabio Broglio, F. Riganti and M. Basile, et al. "Sleep Abnormalities in Type 2 Diabetes may be Associated with Glycemic Control." Acta Diabetol 45 (2008): 225-9.
[Crossref] [Google scholar] [Pubmed]
- Thorp, Alicia A. and Markus P. Schlaich. "Relevance of Sympathetic Nervous System Activation in Obesity and Metabolic Syndrome." J Diabetes Res 2015 (2015): 341583.
[Crossref] [Google scholar] [Pubmed]
- Clarenbach, Christian F., Sophie D. West and Malcolm Kohler. "Is Obstructive Sleep Apnea a Risk Factor for Diabetes?" Discov Med 12 (2011): 17-24.
[Google scholar] [Pubmed]
- Cerón, Elisabet Martínez, Raquel Casitas Mateos and Francisco García-Río. "Sleep Apnea–Hypopnea Syndrome and Type 2 Diabetes. A reciprocal Relationship?" Arch Bronconeumol 51 (2015): 128-39.
[Crossref] [Google scholar] [Pubmed]
- Pallayova, Maria, Ivica Lazurova and Viliam Donic. "Hypoxic Damage to Pancreatic Beta Cells–the Hidden Link between Sleep Apnea and Diabetes." Med Hypotheses 77 (2011): 930-4.
[Crossref] [Google scholar] [Pubmed]
- Doumit, Jimmy and Bharati Prasad. "Sleep Apnea in Type 2 Diabetes." Diabetes Spectr 29 (2016): 14-19.
[Crossref] [Google scholar] [Pubmed]
- Moon, Karoline, Naresh M. Punjabi and R. Nisha Aurora. "Obstructive Sleep Apnea and Type 2 Diabetes in Older Adults." Clin Geriatr Med 31 (2015): 139-47.
[Crossref] [Google scholar] [Pubmed]
- Webb, W. B. and H. W. Agnew. "Are we Chronically Sleep Deprived?" Bull Psychon Soc 6 (1975): 47-48.
- Kent, Brian D., Ludger Grote, Maria R. Bonsignore and Tarja Saaresranta, et al. "Sleep Apnoea Severity Independently Predicts Glycaemic Health in Nondiabetic Subjects: The ESADA Study." Eur Respir J 44 (2014): 130-9.
[Crossref] [Google scholar] [Pubmed]
- Hernandez, Angela, Jacques Philippe and François R. Jornayvaz. "Sleep and Diabetes." Rev Med Suisse 8 (2012): 1198-200.
[Crossref] [Google scholar] [Pubmed]
- Peppard, Paul E., Terry Young, Jodi H. Barnet and Mari Palta, et al. "Increased Prevalence of Sleep-Disordered Breathing in Adults." Am J Epidemiol 177 (2013): 1006-14.
[Crossref] [Google scholar] [Pubmed]
- Kent, Brian D., Walter T. McNicholas and Silke Ryan. "Insulin Resistance, Glucose Intolerance and Diabetes Mellitus in Obstructive Sleep Apnoea." J Thorac Dis 7 (2015): 1343-57.
[Crossref] [Google scholar] [Pubmed]
- Ip, Mary and Babak Mokhlesi. "Sleep and Glucose Intolerance/Diabetes Mellitus." Sleep Med Clin 2 (2007): 19-29.
[Crossref] [Google scholar] [Pubmed]
- Kendzerska, Tetyana, Andrea S. Gershon, Gillian Hawker and George Tomlinson, et al. "Obstructive Sleep Apnea and Incident Diabetes. A Historical Cohort Study." Am J Respir Crit Care Med 190 (2014): 218-25.
[Crossref] [Google scholar] [Pubmed]
- Almendros, Isaac and Francisco García-Río. "Sleep Apnoea, Insulin Resistance and Diabetes: The First Step is in the Fat." Eur Respir J 49 (2017): 1700179.
[Crossref] [Google scholar] [Pubmed]
- Utpat, K., U. Desai, and J. M. Joshi. "Obstructive Sleep Apnea and Diabetes Mellitus: A Bitter Combo." Indian J Sleep Med 13 (2018): 48-52.
- AlDabal, Laila and Ahmed S. BaHammam. "Metabolic, Endocrine, and Immune Consequences of Sleep Deprivation." Open Respir Med J 5 (2011): 31-43.
[Crossref] [Google scholar] [Pubmed]
- Kalsbeek, A., S. Perreauâ?Lenz and R. M. Buijs. "A Network of (Autonomic) Clock Outputs." Chronobiol Int 23 (2006): 521-35.
[Crossref] [Google scholar] [Pubmed]
- Scheer, Frank AJL, Michael F. Hilton, Christos S. Mantzoros and Steven A. Shea. "Adverse Metabolic and Cardiovascular Consequences of Circadian Misalignment." Proc Natl Acad Sci U S A 106 (2009): 4453-8.
[Crossref] [Google scholar] [Pubmed]
- Bolli, Geremia B., Pierpaolo de Feo, Salvatore de Cosmo and Gabriele Perriello, et al. "Demonstration of a Dawn Phenomenon in Normal Human Volunteers." Diabetes 33 (1984): 1150-3.
[Crossref] [Google scholar] [Pubmed]
- Kalsbeek, A., S. Perreauâ?Lenz and R. M. Buijs. "A Network of (autonomic) Clock Outputs." Chronobiol Int 23 (2006): 521-35.
[Crossref] [Google scholar] [Pubmed]
- Fleur, La. "A Suprachiasmatic Nucleus Generated Rhythm in Basal Glucose Concentrations." J Neuroendocrinol 11 (1999): 643-52.
[Crossref] [Google scholar] [Pubmed]
- Ruiter, Marieke, Susanne E. La Fleur, Caroline van Heijningen and Jan van der Vliet, et al. "The Daily Rhythm in Plasma Glucagon Concentrations in the Rat is Modulated by the Biological Clock and by Feeding Behavior." Diabetes 52 (2003): 1709-15.
[Crossref] [Google scholar] [Pubmed]
- Zoccoli, G., T. Cianci, P. Lenzi and C. Franzini. "Shivering During Sleep: Relationship between Muscle Blood Flow and Fiber Type Composition." Experientia 48 (1992): 228-30.
[Crossref] [Google scholar] [Pubmed]
- Morris, Christopher J., Daniel Aeschbach and Frank AJL Scheer. "Circadian System, Sleep and Endocrinology." Mol Cell Endocrinol 349 (2012): 91-104.
[Crossref] [Google scholar] [Pubmed]
- Clore, John N., John E. Nestler and William G. Blackard. "Sleep-Associated Fall in Glucose Disposal and Hepatic Glucose output in Normal Humans: Putative Signaling Mechanism Linking Peripheral and Hepatic Events." Diabetes 38 (1989): 285-90.
[Crossref] [Google scholar] [Pubmed]
- Nutt, David J. "Relationship of Neurotransmitters to the Symptoms of Major Depressive Disorder." J Clin Psychiatry 69 (2008): 4-7.
[Google scholar] [Pubmed]
Citation: AlAmeedy, Waleed Azeez, Taha H. Alnasrawi, Zainab A. Mahdi and Tawfeeq Alghazali, et al. "The Insulin and Glycemic Parameters Role in the Sleep and Depression Disorders in Diabetes Mellitus Type 2 Patients." Clin Schizophr Relat Psychoses 16S (2022). Doi: 10.3371/ CSRP.AWTH.060722.
Copyright: © 2022 AlAmeedy WA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.







 )<6 hours, (
)<6 hours, ( )>6 hours
)>6 hours