Research Article - Clinical Schizophrenia & Related Psychoses ( 2022) Volume 0, Issue 0
The Impact of COVID-19 Pandemic on Quality of Life and Psychological Outcomes Associated Home Quarantine: A Narrative Study
Maryam Bastami1, Hamidreza Monibi2, Elahe Shahamati3 and Ali Yazdanpanah4*2Department International Relations, Rauf Denktaş University, Nicosia, Turkey
3Assistant Master of Clinical Psychology, Department of Psychology and Educational Science, Psychology and Educational Science Research Centre, Islamic Azad University Science and Research Branch, Tehran, Iran
4Assistant Professor, Department of Periodontics, School of Dentistry, Shiraz University of Medical Sciences, Shiraz, Iran
Ali Yazdanpanah, Assistant Professor, Department of Periodontics, School of Dentistry, Shiraz University of Medical Sciences, Shiraz, Iran, Email: ali.yazdanpanah@gmail.com
Received: 16-Dec-2021, Manuscript No. CSRP-21-49940; Editor assigned: 18-Dec-2021, Pre QC No. CSRP-21-49940 (PQ); Reviewed: 01-Jan-2022, QC No. CSRP-21-49940; Revised: 06-Jan-2022, Manuscript No. CSRP-21-49940 (R); Published: 13-Jan-2022, DOI: 10.3371/CSRP.BMHM.011322
Abstract
Background and Aim: One of the important negative effects of the COVID-19 pandemic is the psychological effects and their effects on the quality of life of people in the community. The present study aimed to evaluate the COVID-19 pandemic on quality of life and determine the psychological consequences, based on previous studies and as a review study.
Materials and Methods: To conduct this study, all studies related to the topic under discussion during 2000-2021 by systematic search in internationally available databases, including Web of Science, Science Direct, Scopus, PubMed, and Google Scholar, were checked out. Finally, 41 completely relevant studies were selected to investigate the main objective.
Results: The results showed that pandemic COVID-19 causes anxiety, fear, depression, emotional changes, insomnia, and Post Traumatic Stress Disorder (PTSD) with a high prevalence in the community. In addition, this pandemic significantly affects the quality of life of people compared to the pre-pandemic period.
Conclusion: Based on the study results, it can be concluded that in the COVID-19 pandemic period, it is necessary to identify people prone to psychological disorders at different levels of society whose mental health may be endangered. By providing appropriate psychological strategies and techniques, mental health can be maintained. In addition, health promotion and prevention strategies should be implemented to maintain the mental health of children and adolescents, improve the quality of life, and reduce the burden of COVID-19, especially for children who are most at risk.
Keywords
Coronavirus • Anxiety • Depression • Behavior
Introduction
In December 2019, a respiratory illness caused by a new coronavirus spread in China and has now spread to more than 150 countries [1]. This type of new respiratory disease is characterized by rapid human-tohuman transmission and widespread global epidemics [2]. Crises such as the worldwide epidemic of coronavirus cause a wide range of responses in individuals that affect their physical and mental health [3]. In addition, it concerns public health and causes several psychological problems, including anxiety, fear, depression, labeling, avoidance behavior, irritability, sleep disturbance, and stress [4]. Currently, the COVID-19 pandemic has caused mental health problems worldwide [5]. In a recent study on the prevalence of pandemic COVID-19 in China, people reported mental health problems such as stress (8.1%), anxiety (28.8%), and depression (16.5%) [6].
Due to the pathogenicity of coronavirus, the rate of spread as well as the resulting mortality rate, this disease may affect the mental health status of different people in the community, including patients with COVID-19, health care workers, families, children, students, psychiatric patients and even the staff of other occupations [7-9]. Therefore, during the COVID-19 pandemic, it is essential to identify individuals prone to mental disorders whose mental health may be compromised by exposure to this pandemic.
Although the World Health Organization and public health authorities made great efforts to curb the COVID-19 pandemic before the vaccine was discovered, this massive crisis has caused fear and anxiety worldwide [10]. Early symptoms of the disease included severe pneumonia, fever, muscle aches, and fatigue, followed by consequences such as depression, anxiety, insomnia, and other detrimental psychological effects in patients [11,12]. Clinical anxiety affects up to two-thirds of chronic respiratory patients and reduces their quality of life and physical function [13].
Coronavirus, a chronic respiratory disease with a pandemic prevalence and high mortality rate [14], leads to death in 2% of cases [15]. Preliminary studies have shown that people with underlying diseases and the elderly are at higher risk for morbidity and mortality [16], which can cause anxiety for such people. Furthermore, posttraumatic stress disorder (PTSD) and anxiety can weaken the immune system and make them vulnerable to various diseases such as coronary heart disease [13]. In addition, numerous studies have shown that life events can affect psychological well-being [17- 20].
Psychological well-being is a sense of satisfaction from the perspective of social psychologists [21], which means well-being and happiness and achieving full potential, and includes life satisfaction, positive and negative emotions, as well as happiness [22]. Since psychological well-being has many positive psychological consequences, it is essential to study the factors affecting this factor [21]. Anxiety caused by the COVID-19 pandemic is a sudden event that can disrupt individuals and society's psychological well-being and quality of life. Therefore, the purpose of this review is to investigate the effect of the COVID-19 pandemic on the quality of life and the mental health of people in the community.
Materials and Methods
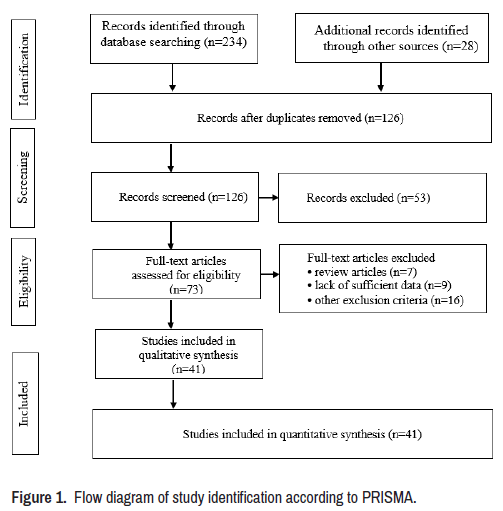
The present study aimed to investigate the effect of the COVID-19 pandemic on quality of life and mental health in the community. For this purpose, systematic searches of internationally available databases including Web of Science, Science Direct, Scopus, PubMed, and Google Scholar were performed between 2000 and 2021. Systematic review carried out by using Mesh terms "COVID-19", "Pandemic", "Quality of Life", "Psychological well-being", "Psychological Outcomes", "Home Quarantine", "Mental Health" and "Psychological Effect", "Anxiety", "Patients", "QoL", "Health-Related Quality of Life" and "HRQoL". For other databases, the same mesh terms were used similarly. The references were thoroughly evaluated to verify that no articles were missed for inclusion in the study (Reference Checking). In addition, the citations from the research were also checked (Citation Tracing) to make sure that the search was thorough and successful. According to Figure 1, the search for literature, especially articles, was done according to the PRISMA guideline [23]. In addition, unofficial reports, articles in a letter to editor format, and unpublished articles and content posted on Internet sites were removed from the list of downloaded files. Finally, the results of 41 published articles were reviewed for the present review.
Results and Discussion
Mental health of COVID-19 patients
COVID-19 has a unique feature because it has spread to all world countries due to its very high spread in less than a few months and creating a pandemic situation [24,25]. Early in the pandemic, the number of patients with the disease and the resulting mortality increased rapidly worldwide [26,27]. Based on this and considering the emergency of this disease, it is predictable that some symptoms of psychological disorders will occur in patients with COVID-19. In this regard, the results of several studies on patients with COVID-19 in China, some of these psychological disorders, including anxiety, fear, depression, emotional changes, insomnia, and Post Traumatic Stress Disorder (PTSD), with high prevalence in these patients has been reported [28,29].
Rapid release of COVID-19 isolated patients in the intensive care unit with acute respiratory problems, lack of effective drug treatment, and mortality from this disease are the most important factors affecting the mental health of people with this disease [30-32]. According to some previous studies, COVID-19 patients have a low psychological tolerance capacity, and due to the current state of the disease in the world, people are highly exposed to psychological disorders such as anxiety, fear, depression, and negative thoughts [33]. PTSD is one of the most important psychological disorders that can damage patients' mental health with COVID-19 [32]. If this psychological disorder is not controlled, it may lead to permanent injuries in patients such as intrusive memories, avoidant behaviors, irritability, and emotional numbing [32,34].
PTSD is a stress-related psychological problem that occurs in people who experience a life-threatening condition [35]. According to available sources, the experience of life-threatening physical illnesses such as COVID-19 can cause PTSD symptoms [34]. Sleep disturbance is another problem for people with COVID-19 that may occur in isolated or quarantined wards. The results of a study in China during the publication of COVID-19 disease in Wuhan show that the sleep quality index in these patients decreases sharply [36]. On the other hand, the results of this study show a relationship between sleep quality disorders and the occurrence of psychological disorders such as PTSD. Anxiety and depression are other important psychological disorders that can damage the mental health of patients with COVID-19. The results of Yang et al. study conducted on patients admitted to a Chinese hospital included 143 participants, including 21 infected with COVID-19, 86 with pneumonia, and 30 healthy. This study shows that the assessment index of anxiety and depression in patients with respiratory problems (patients with COVID-19 and pneumonia) is higher than in healthy people. In addition, both depression and anxiety indices are significantly higher in people infected with COVID-19 than in people with pneumonia [28]. Because these people, in addition to receiving medical services to treat their physical illness, also need psychological interventions, the use of psychological interventions based on the results of this study has significantly reduced both anxiety and depression in COVID-19 patients.
Mental health of quarantined people due to being infected with COVID-19
Quarantine means isolating and restricting the movement of people who are potentially exposed to a contagious disease to prevent the infection of other people in the community if the disease is identified [37]. The definition of quarantine is completely different from isolation because isolation means isolating people who have been diagnosed with an infectious disease and must be separated from people who are not sick [37]. During the quarantine process, depending on the environmental conditions and the type of infectious disease spread, people's mental health may be damaged, and some psychological disorders may occur in people in quarantine [38]. In general, all studies that have evaluated the psychological disorders of quarantined individuals reported many signs of psychological damage such as emotional distress, depression, stress, mood swings, mobility, insomnia, decreased attention, PTSD, anger, and emotional numbness [37-39]. The study of Bai et al., performed on hospital staff after a 9-day quarantine period due to contact with people infected with the SARS virus, showed signs of acute stress disorder [40]. This study also found that quarantine personnel showed signs of fatigue, isolation, anxiety when working with feverish people, irritability, insomnia, decreased ability to decide and concentrate, and reduced performance quality.
The results of Wang et al. study show that PTSD is an important psychological symptom that has been observed in various quarantined individuals due to infectious influenza in hospital staff [38]. It is noteworthy that PTSD symptoms are about four times higher among quarantined children than non-quarantined children, which indicates the occurrence of psychological symptoms with a higher proportion of children than adults [41].
Depression is another symptom of mental health disorder in patients and hospital staff after quarantine. According to the results of Liua et al. study, about 9% of people and hospital staff showed severe symptoms of depression three years after quarantine [42]. During the spread of COVID-19, quarantine is the most common and best strategy to prevent the spread of the disease [39]. According to previous studies, the most common triggers for stress and psychological disorders in quarantined people due to COVID-19 include fear of infecting themselves or others, long period of quarantine, inadequate support and lack of Adequate access to medical care and food, and ultimately fatigue and boredom due to quarantine and isolation have been reported. All of the above, as well as the addition of some unpleasant thoughts such as loneliness, stigmatization, denial, despair, and in more severe degrees of aggression and suicidal thoughts, may put the patient in quarantine for COVID-19, reduce adherence to continued treatment, and even people intend to leave the quarantine site. Finally, quarantine conditions cause individuals to lose the psychological support of family and friends, which in turn exacerbates stress and psychological damage [43].
Mental health of students in during COVID-19 pandemic
School closures and home quarantine due to the spread of infectious diseases such as COVID-19 affect children and adolescents' physical and mental health [44,45]. The results of Mason et al. showed that children and adolescents, when are on weekends or summer vacations, do less physical activity, their sleep pattern is impaired, and they do not follow a proper diet [46]. This phenomenon is exacerbated when children are confined to the home and do not engage in outdoor activities. On the other hand, the emergence of stressful stimuli at home such as long-term fear of getting COVID-19, unpleasant thoughts and boredom, lack of communication with classmates, friends, and teachers, lack of adequate space at home, and financial and economic problems of parents can have lasting effects on the mental health of children and adolescents [37]. It is noteworthy that according to Shahyad et al. the average PTSD index in quarantined children is four times that of non-quarantined children. Therefore, children who are isolated or quarantined due to their current condition (COVID-19) will definitely show more severe psychological symptoms, such as acute stress disorder, adjustment disorder. According to related reports, 30% of these children show symptoms of PTSD [43].
University students are another person prone to developing psychological symptoms during the outbreak of COVID-19. At the beginning of the disease outbreak in the world, the closure of universities was one of the first and most basic solutions to prevent the widespread of COVID-19. According to a study conducted during the H1N1 flu pandemic in China in 2009, about 2% of college students experience symptoms of PTSD [47]. According to a study conducted in China on more than 7,000 students during the publication of COVID-19, the results indicate that about 24.9% of students have experienced anxiety. About 9 people reported symptoms of severe anxiety, and the rest reported mild anxiety. One of the most important causes of anxiety among students is worrying about the impact of the COVID-19 virus on their future education, future employment status, and reduced social connections. Anxiety in some students may also be a problem in providing university tuition due to financial resources due to unemployment and job loss. Accordingly, having a stable family income, living in urban areas, and living with the family are one of the most important factors in reducing anxiety among students. According to the findings of Cao et al. and Fakari and Simbar studies, the incidence of COVID-19 in relatives and acquaintances is another cause of anxiety among students [48,49].
Mental health of the general public
Since the beginning of the COVID-19 pandemic, the disease was new and unknown, and after a few months, no effective treatment and vaccine were found. Therefore, during the spread of COVID-19, keeping different people in the community at home (social distance) is the most common and best strategy to prevent the spread of the disease [43]. Accordingly, different psychological disorders may be observed among various family members due to people staying at home. The results of Xiao et al. study found that sleep quality in people who isolated themselves for 14 days during the release of COVID-19 in China in January 2020 show that sleep disorders are associated with increased anxiety and stress in these people, which can be addressed with appropriate social support, improved sleep quality in these patients [50]. Another study conducted by Sun et al. in early 2020 among ordinary people after the release of COVID-19 in China shows that out of about 2019 participants who participated in this study online, about 4.6% of people with high rates of PTSD have been reported [34]. Some of the factors that seem to affect the onset of psychological symptoms in the general public include concerns about the risk of disease, future employment status and sources of income for individuals and families, and the long period of home quarantine [43].
Effect of COVID-19 on quality of life
The term "health-related quality of life" (HRQoL) refers to the degree of well-being that results from an individual's assessment of multiple aspects of his/her life, keeping in mind that these aspects influenced their health status (e.g., physical, mental, and social well-being). It is characterized as being personal, diverse, and altering throughout the life span [51]. The HRQoL assessment evaluates the ability to participate in activities fully and perform physical, social, and psychosocial functions relevant to their age early, based on evolutionary development and individual characteristics within a given cultural environment. Children who have a poor HRQoL are less likely to grow to be healthy adults [52].
Several children and adolescents in developed nations lead inactive lifestyles, participate in fewer physical leisure activities, and become more reliant on sedentary lifestyles [53]. For example, in a study conducted before the COVID-19 pandemic, it was shown that 81% of students between the ages of 11 and 17 were partly functionally active [54]. Sedentary activities, mainly those reliant on electric appliances, are linked to an improved risk of obesity, a decline in body function, self-confidence, and prosocial behavior, regardless of sports participation [55]. In this approach, the COVID-19 pandemic has raised the sum of screen leisure time [56,57]. This is quite relevant since a previous systematic review showed that the evidence for screen time linked with lower HRQoL was moderate [58].
Besides inactivity, stressful conditions, including the COVID-19 pandemic, have influenced the children's HRQoL. House isolation circumstances and the internet or mobile phone use have also been effective in creating these conditions. The COVID-19 pandemic has led to rapid, unusual modifications to the lives of billions of children and adolescents [59,60].
A sum of 3177 children and adolescents throughout COVID-19 were involved in the systematic review of Nobari et al. In this study, 3 papers revealed that the COVID-19 pandemic substantially affected the children and adolescents' HRQoL. On the other hand, another did not record a correlation between pre-and during the COVID-19 pandemic; though, a reduction in the HRQoL can be seen. Nonetheless, 2 papers did not find significant changes, and another one did not report p-values. Moreover, about sex variations, only 2 studies investigated this point, seeing no variations amid males and females in the influence of the COVID-19 pandemic on HRQoL. Considering that, this systematic review might confirm that COVID-19 harms the HRQoL of children and adolescents [61].
Ferreira et al. determined that people with home isolation had higher stress and lower HRQoL levels and that people with more anxiety led to having a lower HRQoL. According to the results of this study, women and adult persons encountered the highest levels of stress and lower HRQoL. Furthermore, HRQoL throughout the quarantine can be described by several official and attitudinal variables and sociodemographic variables [62].
Kharshiing et al. reported that Quality of Life (QoL) was substantially affected by personal variables (COVID-19 anxiety and individual status) and group variables (family and community identification). The effect of COVID-19 stress and unique personality as private variables is over and above demographic variables on QoL. Group variables (family and country description) significantly impacted QoL over and above the personal variables [63]. Based on the results of the Ravens-Sieberer et al. study in Germany, 2/3 of the children and adolescents described being highly burdened by the COVID-19 pandemic. As a result, they encountered considerably lower HRQoL (40.2% vs. 15.3%), more mental health problems (17.8% vs. 9.9%), and higher anxiety levels (24.1% vs. 14.9%) than before the pandemic. Moreover, children with low socioeconomic status, migration background, and limited living space were significantly affected [64].
Consequently, people with mental health should be taken into attention throughout pandemics or extra emergencies. Stress and other factors can reduce an individual's HRQoL related to the pandemic's cultural and financial outcomes.
Conclusion
The release of COVID-19, due to the rapid transmission of the virus, has created a global health emergency in less than a few months around the world. This contagious disease raises concerns about public physical health and causes many psychological illnesses. In this situation, it is essential to maintain people's mental health because people in different parts of society may experience stressful stimuli during the release of COVID-19. Therefore, in the current high-risk situation, identifying people prone to psychological disorders at different levels of society whose mental health may be endangered is essential to maintain mental health with appropriate psychological strategies and techniques. Furthermore, health promotion and prevention strategies should be implemented to maintain the mental health of children and adolescents, improve HRQoL, and reduce the burden of COVID-19, especially for children who are most at risk.
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- Porcheddu Rossella, Serra Caterina, Kelvin David and Kelvin Nikki, et al. “Similarity in Case Fatality Rates (CFR) of COVID-19/SARS-COV-2 in Italy and China.” J Infect Dev Ctries 14 (2020): 25-28.
[Crossref] [Google Scholar] [Pubmed]
- Yu, Jing, Wen Ouyang, Melvin LK Chua and Conghua Xie. “SARS-CoV-2 Transmission in Patients with Cancer at a Tertiary care Hospital in Wuhan, China.” JAMA 6 (2020): 1108-1110.
[Crossref] [Google Scholar] [Pubmed]
- Shahyad SH and Mohammadi MT. “Psychological Impacts of Covid-19 Outbreak on Mental Health Status of Society Individuals: A Narrative Review.” J Military Med 22 (2020):184-92.
- Chen, Nanshan, Min Zhou, Xuan Dong and Jieming Qu, et al. “Epidemiological and Clinical Characteristics of 99 Cases of 2019 Novel Coronavirus Pneumonia in Wuhan, China: A Descriptive Study.” Lancet 395 (2020): 507-513.
[Crossref] [Google Scholar] [Pubmed]
- Wang, Cuiyan, Riyu Pan, Xiaoyang Wan and Yilin Tan et al. “A Longitudinal Study on the Mental Health of General Population During the COVID-19 Epidemic in China.” Brain Behav Immun 87 (2020): 40-48.
[Crossref] [Google Scholar] [Pubmed]
- Liang, Wenhua, Weijie Guan, Ruchong Chen and Wei Wang, et al. “Cancer Patients in SARS-CoV-2 Infection: A Nationwide Analysis in China.” Lancet Oncol 21 (2020): 335-337.
[Crossref] [Google Scholar] [Pubmed]
- Bao, Yanping, Yankun Sun, Shiqiu Meng and Jie Shi, et al. “2019-nCoV Epidemic: Address Mental Health Care to Empower Society.” Lancet 395 (2020): e37-e38.”
[Crossref] [Google Scholar] [Pubmed]
- Ryu, Sukhyun, Byung Chul Chun and Korean Society of Epidemiology. “An Interim Review of the Epidemiological Characteristics of 2019 Novel Coronavirus.” Epidemiol Health 42 (2020): 1-2.
[Crossref] [Google Scholar] [Pubmed]
- Chen, Qiongni, Mining Liang, Yamin Li and Jincai Guo, et al. “Mental Health Care for Medical Staff in China During the COVID-19 Outbreak.” Lancet Psychiatry 7 (2020): e15-e16.
[Crossref] [Google Scholar] [Pubmed]
- Fathi, Ayatollah, Solmaz Sadeghi, Ali Akbar Maleki Rad and Hossein Rostami, et al. “Effect of Health-Promoting Lifestyle and Psychological Well-Being on Anxiety Induced by Coronavirus Disease 2019 in Non-Medical Students.” J Arak University Med Sci 23 (2020): 698-709.
- Liu, Nianqi, Fan Zhang, Cun Wei and Yanpu Jia, et al. “Prevalence and Predictors of PTSS During COVID-19 Outbreak in China Hardest-Hit Areas: Gender Differences Matter.” Psychiatry Res 287 (2020): 112921.
- Lai, Jianbo, Simeng Ma, Ying Wang and Zhongxiang Cai, et al. “Factors Associated with Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019.” JAMA Netw Open 3 (2020): e203976-e203976.
[Crossref] [Google Scholar] [Pubmed]
- Alipour Ahmad, Ghadami Abolfazl, Alipour Zahra and Abdollahzadeh Hasan. “Preliminary Validation of the Corona Disease Anxiety Scale (CDAS) in the Iranian Sample. Quarterly J Health Psychology 8 (2020):163-75.
- Kooraki, Soheil, Melina Hosseiny, Steven S Raman and Lee Myers, et al. “Coronavirus Disease 2019 (COVID-19) Precautions: What the MRI Suite Should Know.” J Am Coll Radiol 17 (2020): 830.
[Crossref] [Google Scholar] [Pubmed]
- Fard SA, Saffarinia Majid. “The Prediction of Mental Health Based on the Anxiety and the Social Cohesion that Caused by Coronavirus.” Soc Psychol Res 9 (2020): 129-41. [Crossref]
- Tavakoli Ahmad, Vahdat Katayon and Keshavarz Mohsen. “Novel Coronavirus Disease 2019 (COVID-19): An Emerging Infectious Disease in the 21st Century.” ISMJ 22 (2020): 432-50.
- Mohammadpour S and Jooshanlou M. “Relationship between Published Anxiety Disorder and Obsessive-Compulsive Personality Disorder with Psychological Well-Being of Students of Lorestan University of Medical Sciences in 2014: The Mediating Role of Passionate Obsessive Love Persian.” J Rafsanjan Univ Med Sci 14 (2015): 353-66.
- Bahadori Khosroshahi, Jafar and Toraj Hashemi Nosrat Abad T. “The Relationship between Social Anxiety, Optimism and Self-Efficacy with Psychological Well-Being in Students.” Studies Med Sci 23 (2012): 115-122.
- Esmaeili, Shiva, Afsaneh Ghanbari Panah and Roya KoochakEntezar. “Prediction of Psychological Well-being Based on Perceived Health Anxiety and Stress with its Mediating Role of Disability in Married Women Working in the School of Nursing and Midwifery, Tehran University of Medical Sciences in 2018.” Iran J Nurs Res 14 (2020): 46-52.
- Freire, Carlos, María Del Mar Ferradás, Antonio Valle and José C Núñez, et al. “Profiles of Psychological Well-Being and Coping Strategies Among University Students.”Front Psychol 7 (2016): 1554.
[Crossref] [Google Scholar] [Pubmed]
- Hatefnia Fateme, Dortaj Fariborz, Alipour Ahmad, Farokhi Noor Ali. “The Effect of Academic Procrastination on Psychological well-being: The Mediating Role of Floating, Positive-Negative Emotions and Life Satisfaction (Persian).” Soc Psychol Res 9 (2019):53-76. [Crossref] [Google Scholar] [Pubmed]
- Ghazavi, Z, R Zeighami, ME Sarichello, and S Shahsavari. “Effective Training of Cognitive Regulation Strategies on the Psychological Well-being of Nurses Working in Psychiatric Wards.” Iran J Psychiatry 7 (2019): 64-73. [Crossref]
[Google Scholar] [Pubmed]
- Moher, David, Alessandro Liberati, Jennifer Tetzlaff and Douglas G Altman. “Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement.” Int J Surg 8 (2010): 336-341.
[Crossref] [Google Scholar] [Pubmed]
- Liu, Xia, RS Narisa and Zhenqiang. “Challenges to Prevent and Control the Outbreak of COVID-19.” Zhonghua Liu Xing Bing Xue Za Zhi 41 (2020): 994-997. [Crossref]
[Google Scholar] [Pubmed]
- Zhao, Shilei and Hua Chen. “Modeling the Epidemic Dynamics and Control of COVID-19 Outbreak in China.” Quant Biol 8 (2020): 11-19.
[Crossref] [Google Scholar] [Pubmed]
- Zangrillo, Alberto, Luigi Beretta, Anna Mara Scandroglio and Giacomo Monti, et al. “Characteristics, Treatment, Outcomes and Cause of Death of Invasively Ventilated Patients with COVID-19 ARDS in Milan, Italy.” Crit Care Resusc 22 (2020): 200-211. [Crossref]
[Goggle Scholar] [Pubmed]
- Remuzzi, Andrea and Giuseppe Remuzzi. “COVID-19 and Italy: What Next?.” Lancet 395 (2020): 1225-1228.
[Crossref] [Goggle Scholar] [Pubmed]
- Yang, Lu, Danjuan Wu, Yanbin Hou and Xunqiang Wang, et al. “Analysis of Psychological State and Clinical Psychological Intervention Model of Patients with COVID-19.” MedRxiv 2020 (2020): 1-8.
[Crossref] [Goggle Scholar] [Pubmed]
- Liu, Shuai, Lulu Yang, Chenxi Zhang and Yu-Tao Xiang, et al. “Online Mental Health Services in China During the COVID-19 Outbreak.” Lancet Psychiatry 7 (2020): e17-e18.
[Crossref] [Goggle Scholar] [Pubmed]
- Xiang, Yu-Tao, Yuan Yang, Wen Li and Ling Zhang, et al. “Timely Mental Health Care for the 2019 Novel Coronavirus Outbreak is Urgently Needed.” Lancet Psychiatry 7 (2020): 228-229.
[Crossref] [Goggle Scholar] [Pubmed]
- Lima, Carlos Kennedy Tavares, Poliana Moreira de Medeiros Carvalho, Igor de Araújo Araruna Silva Lima and José Victor Alexandre de Oliveira Nunes, et al. “The Emotional Impact of Coronavirus 2019-nCoV (new Coronavirus disease).” Psychiatry Res 287 (2020): 112915.
[Crossref] [Goggle Scholar] [Pubmed]
- Bo, Hai-Xin, Wen Li, Yuan Yang and Yu Wang, et al. “Posttraumatic Stress Symptoms and Attitude Toward Crisis Mental Health Services Among Clinically Stable Patients with COVID-19 in China.” Psychol Med 51 (2021): 1052-1053.
[Crossref] [Goggle Scholar] [Pubmed]
- Yao, Hao, Jian-Hua Chen and Yi-Feng Xu. “Patients with Mental Health Disorders in the COVID-19 Epidemic.” 7 (2020): 1-1.
[Crossref] [Goggle Scholar] [Pubmed]
- Sun, Luna, Zhuoer Sun, Lili Wu and Zhenwen Zhu, et al. “Prevalence and Risk Factors of Acute Posttraumatic Stress Symptoms during the COVID-19 Outbreak in Wuhan, China.” MedRxiv (2020): 1-17.
[Crossref] [Goggle Scholar] [Pubmed]
- Kessler, Ronald C. “Posttraumatic Stress Disorder: The Burden to the Individual and to Society.” J Clin Psychiatry 61 (2000): 4-14. [Crossref]
[Goggle Scholar] [Pubmed]
- Zhang, Fan, Zhilei Shang, Haiying Ma and Yanpu Jia, et al. “High Risk of Infection Caused Posttraumatic Stress Symptoms in Individuals with Poor Sleep Quality: A Study on Influence of Coronavirus Disease (COVID-19) in China.” MedRxiv 2020 (2020): 1-13.
[Crossref] [Goggle Scholar] [Pubmed]
- Brooks, Samantha K, Rebecca K Webster, Louise E Smith and Lisa Woodland, et al. “The Psychological Impact of Quarantine and How to Reduce it: Rapid Review of the Evidence." Lancet 395 (2020): 912-920.
[Crossref] [Goggle Scholar] [Pubmed]
- Wang, Yongguang, Baihua Xu, Guoqiu Zhao and Rifang Cao, et al. “Is Quarantine Related to Immediate Negative Psychological Consequences During the 2009 H1N1 Epidemic?” Gen Hosp Psychiatry 33 (2011): 75-77.
[Crossref] [Goggle Scholar] [Pubmed]
- Rubin G James, Wessely Simon. “The Psychological Effects of Quarantining a City.” BMJ 2020 (2020): 368.
[Crossref] [Goggle Scholar] [Pubmed]
- Bai, YaMei, Chao-Cheng Lin, Chih-Yuan Lin and Jen-Yeu Chen, et al. “Survey of Stress Reactions Among Health Care Workers Involved with the SARS Outbreak.” Psychiatr Serv 55 (2004): 1055-1057.
[Crossref] [Goggle Scholar] [Pubmed]
- Robertson, Emma, Karen Hershenfield, Sherry Lynn Grace and Donna Eileen Stewart. “The Psychosocial Effects of Being Quarantined Following Exposure to SARS: A Qualitative Study of Toronto Health care Workers.” Can J Psychiatry 49 (2004): 403-407.
[Crossref] [Goggle Scholar] [Pubmed]
- Liua, Xinhua, Meghana Kakadeb, Cordelia J Fullerb and Bin Fanb, et al. “Depression After Exposure to Stressful Events: Lessons Learned from the SARS Epidemic.” Compr Psychiatry 53 (2012): 15-23.
[Crossref] [Goggle Scholar] [Pubmed]
- Shahyad, Shima and Mohammad Taghi Mohammadi. “Psychological Impacts of Covid-19 Outbreak on Mental Health Status of Society Individuals: A Narrative Review.” J Military Med 22 (2020): 184-192. [Crossref]
[Goggle Scholar] [Pubmed]
- Wang, Guanghai, Yunting Zhang, Jin Zhao and Jun Zhang, et al. “Mitigate the Effects of Home Confinement on Children During the COVID-19 Outbreak.” Lancet 395 (2020): 945-947.
[Crossref] [Goggle Scholar] [Pubmed]
- Sprang, Ginny and Miriam Silman. "Posttraumatic Stress Disorder in Parents and Youth after Health-Related Disasters.” Disaster Med Public Health Prep 7 (2013): 105-110.
[Crossref] [Goggle Scholar] [Pubmed]
- Mason, Frances, Amanda Farley, Miranda Pallan and Alice Sitch, et al. “Effectiveness of a Brief Behavioural Intervention to Prevent Weight Gain over the Christmas Holiday Period: Randomised Controlled Trial.” BMJ 363 (2018).
[Crossref] [Goggle Scholar] [Pubmed]
- Xu, Jiahong, Yayuan Zheng, Mingmin Wang and Jiangmin Zhao, et al. “Predictors of Symptoms of Posttraumatic Stress in Chinese University Students During the 2009 H1N1 Influenza Pandemic.” Med Sci Monit 17 (2011): PH60.
[Crossref] [Goggle Scholar] [Pubmed]
- Cao, Wenjun, Ziwei Fang, Guoqiang Hou and Mei Han, et al. “The Psychological Impact of the COVID-19 Epidemic on College Students in China.” Psychiatry Res 287 (2020): 112934.
[Crossref] [Goggle Scholar] [Pubmed]
- Fakari, Farzaneh Rashidi and Masoumeh Simbar. “Coronavirus Pandemic and Worries During Pregnancy; a Letter to Editor.” Arch Acad Emerg Med 8 (2020): e21-e21. [Crossref]
[Goggle Scholar] [Pubmed]
- Xiao, Han, Yan Zhang, Desheng Kong and Shiyue Li, et al. “Social Capital and Sleep Quality in Individuals Who Self-isolated for 14 days During the Coronavirus Disease 2019 (COVID-19) Outbreak in January 2020 in China.” Med Sci Monit 26 (2020): e923921-1.
[Crossref] [Goggle Scholar] [Pubmed]
- Whoqol Group. “The World Health Organization Quality of Life Assessment (WHOQOL): Position Paper from the World Health Organization.” Soc Sci Med 41 (1995): 1403-1409.
[Crossref] [Goggle Scholar] [Pubmed]
- Riley, Anne W, Georg Spiel, David Coghill and Manfred Döpfner, et al. “Factors Related to Health-Related Quality of Life (HRQoL) Among Children with ADHD in Europe at Entry into Treatment.” Eur Child Adolesc Psychiatry 15 (2006): 38-45.
[Crossref] [Google Scholar] [Pubmed]
- Gopinath, Bamini, Louise L Hardy, Louise A Baur and George Burlutsky, et al. “Physical Activity and Sedentary Behaviors and Health-related Quality of Life in Adolescents.” Pediatrics 130 (2012): e167-e174.
[Crossref] [Google Scholar] [Pubmed]
- Guthold, Regina, Gretchen A Stevens, Leanne M Riley and Fiona C Bull. “Global Trends in Insufficient Physical Activity Among Adolescents: A Pooled Analysis of 298 Population-Based Surveys with 1·6 Million Participants.” Lancet Child Adolesc Health 4 (2020): 23-35.
[Crossref] [Google Scholar] [Pubmed]
- Tremblay, Mark S, Allana G LeBlanc, Michelle E Kho and Travis J Saunders, et al. “Systematic Review of Sedentary Behaviour and Health Indicators in School-Aged Children and Youth.” Int J Behav Nutr Phys Act 8 (2011): 1-22.
[Crossref] [Google Scholar] [Pubmed]
- López-Bueno, Rubén, Guillermo Felipe López-Sánchez, José A Casajús and Joaquín Calatayud, et al. “Health-related Behaviors Among School-aged Children and Adolescents During the Spanish Covid-19 Confinement.” Front Pediatr 47 (2020): 573. [Crossref]
[Google Scholar] [Pubmed]
- Xiang, Mi, Zhiruo Zhang and Keisuke Kuwahara. “Impact of COVID-19 Pandemic on Children and Adolescents' Lifestyle Behavior Larger than Expected.” Prog Cardiovasc Dis 63 (2020): 531.
[Crossref] [Google Scholar] [Pubmed]
- Stiglic, Neza and Russell M Viner. “Effects of Screentime on the Health and Well-being of Children and Adolescents: A Systematic Review of Reviews.” BMJ Open 9 (2019): e023191.
[Crossref] [Google Scholar] [Pubmed]
- Chtourou, Hamdi, Khaled Trabelsi, Cyrine H'mida and Omar Boukhris, et al. “Staying Physically Active During the Quarantine and Self-isolation Period for Controlling and Mitigating the COVID-19 Pandemic: A Systematic Overview of the Literature.” Front Psychol 11 (2020): 1708.
[Crossref] [Google Scholar] [Pubmed]
- Fazeli, Sara, Isa Mohammadi Zeidi, Chung-Ying Lin and Peyman Namdar, et al. “Depression, Anxiety, and Stress Mediate the Associations Between Internet Gaming Disorder, Insomnia, and Quality of Life During the COVID-19 Outbreak.” Addict Behav Rep 12 (2020): 100307.
[Crossref] [Google Scholar] [Pubmed]
- Nobari, Hadi, Mohamad Fashi, Arezoo Eskandari and Santos Villafaina, et al. “Effect of COVID-19 on Health-Related Quality of Life in Adolescents and Children: A Systematic Review.” Int J Environ Res Public Health 18 (2021): 4563.
[Crossref] [Google Scholar] [Pubmed]
- Ferreira, Lara N, Luís N Pereira, Maria da Fé Brás and Kateryna Ilchuk. “Quality of Life Under the COVID-19 Quarantine.” Qual Life Res 30 (2021): 1389-1405.
[Crossref] [Google Scholar] [Pubmed]
- Kharshiing, Korsi Dorene, Drishti Kashyap, Kaveri Gupta and Masrat Khursheed, et al. “Quality of Life in the COVID-19 Pandemic in India: Exploring the Role of Individual and Group Variables.” Community Ment Health J 57 (2021): 70-78.
[Crossref] [Google Scholar] [Pubmed]
- Ravens-Sieberer, Ulrike, Anne Kaman, Michael Erhart and Janine Devine, et al. “Impact of the COVID-19 Pandemic on Quality of Life and Mental Health in Children and Adolescents in Germany.” Eur Child Adolesc Psychiatry 25 (2021): 1-11.
[Crossref] [Google Scholar] [Pubmed]
Citation: Bastami, Maryam, Hamidreza Monibi, ElaheShahamati and Ali Yazdanpanah. "The Impact of COVID-19 Pandemic on Quality of Life and Psychological Outcomes Associated Home Quarantine-A Narrative Reviewed." Clin Schizophr Relat Psychoses 16S (2022). DOI: 10.3371/CSRP.BMHM.011322.
Copyright: © 2022 Bastami M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.