Brief Report - Clinical Schizophrenia & Related Psychoses ( 2022) Volume 0, Issue 0
The Effect of Sleep in Serotonin Level for Different Duration Periods of Depression Disorders
Allaa Hatim Thanoon1, Mohammed Abed Jawad2*, Mohammed Haider Hamad3, Mohammed Shakir Atiyah4, Saif Yaseen Hasan5, Ahlam Kadhim Hussein6, Doaa A Hamad7, Falah Hassan Ali8 and Ghadeer Sabah Bustani92Department of Medicine, Al‐Nisour University, Baghdad, Iraq
3Department of Medical Laboratory, Al Mustaqbal University, Babylon, Iraq
4Department of Medical Sciences, Al‐Manara College, Maysan, Iraq
5Department of Medical Sciences, National University of Science and Technology, Dhi‐Qar, Iraq
6Department of Nursing, Al‐Zahrawi University College, Karbala, Iraq
7Department of Nursing, Hilla University, Babylon, Iraq
8Department of Medical Sciences, Al‐Esraa University College, Baghdad, Iraq
9Department of Medical Sciences, The Islamic University, Najaf, Iraq
Mohammed Abed Jawad, Department of Medicine, Al‐Nisour University, Baghdad, Iraq, Email: mohammed.a.medical.lab@nuc.edu.iq
Received: 08-Nov-2021, Manuscript No. CSRP-21-46861; Editor assigned: 10-Nov-2021, Pre QC No. CSRP-21-46861 (PQ); Reviewed: 24-Nov-2021, QC No. CSRP-21-46861; Revised: 02-Dec-2021, Manuscript No. CSRP-21-46861 (R); Published: 10-Dec-2021, DOI: 10.3371/CSRP. TAMJ.121022
Abstract
The current study deal with effect of sleep in serotonin level in a different duration period of depressed patients, blood sample collected from depression patients then serotonin detected, the results show non-significant serotonin level (P=0.566) and sleep show a significant decrement in patients than control (p=0.000), significant differences among sleep categories distribution (p=0.0012), The mean differences in serotonin level according to sleep categories show non -significant differences within the depression patient groups (p=0.110) and control groups (p=0.439), there was non-significant differences among duration categories for serotonin level (P=0.217) and sleep (P=0.335) , there wasn't relation of serotonin level with sleep in different disease duration. Also serotonin decreased during the period (5-10 years) while increasing after (10 years) of disease. Present study concluded that serotonin affected by sleep in depression and didn’t effect by duration of disease, sleep decrease with duration increment.
Keywords
Serotonin • Sleep • Depression • Disorder
Introduction
The disrupted sleep is an important problem in population in the last years, the lifestyle and increased work pressure, and psychosocial stress, the long term of insufficient sleep may be led to various diseases including psychiatric disorders [1-6]. The sleep disturbance has been found to be associated with symptoms of the disease, some investigations proposed that the relationship between mood disorders and sleep is more complex [7,8] .
Serotonin is one of the neurotransmitter in the central nervous system contributed to a wide range of behavioural, pathological and physiological processes [9], the role of serotonin in the wakefulness-sleep cycle isn’t fully understood, however, its contributed in an emotional reaction, the inactivation of serotonin associated with diseases as well as depression, anxiety and schizophrenia disorders, etc. that characterized by sleep disorder [10,11] . The linked among depression, sleep and serotonin level was suggested in the present study in different duration of depression disordered disease.
Methodology
The Present study included depression patients that attended to a psychiatric clinic, and diagnosed as a major depression disorders by psychiatric physician, patients have age ranged (20-60 year) and BMI (16- 32 Kg/m2). Control group included healthy individuals have age ranged (22-60 year) and BMI (18-32 Kg/m2) were enrolled in the present study, data and blood samples were collected with written consents from all contributors in the study. The data consists of age, BMI, sleep, disease duration.
Exclusion criteria: Diabetes mellitus, cancer, viral infection disease, cardiovascular disease and hormonal disturbance.
Serotonin level was detected using ELIZA technique, then data analyzed used SPSS V23, independent t test, correlation coefficient were using at P value<0.05.
Results and Discussion
Current output exhibits in Table 1 that shows non-significant serotonin level (P=0.566) and sleep show a significant decrement in patients than control (p=0.000).
| Study variables | Control group | Depression patients | Sig |
|---|---|---|---|
| Duration | 7.6632 ± 1.738 | - | - |
| Sleep | 4.4737 ± 0.632 | 7.7895 ± 0.363 | 0.000 |
| Serotonin | 54.3464 ± 3.790 | 62.2353 ± 13.077 | 0.566 |
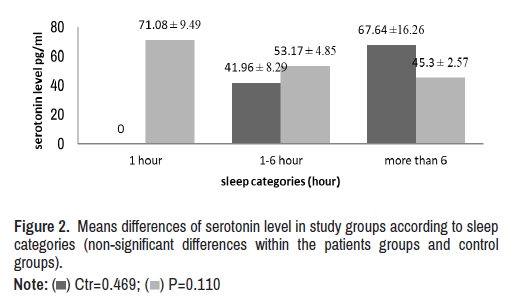
Three categories of sleep were depended in present study 1 hour, 1-6 hour and more than 6 hours, there were significant differences among sleep categories distribution (X2=13.368, p=0.0012) (Figure 1).
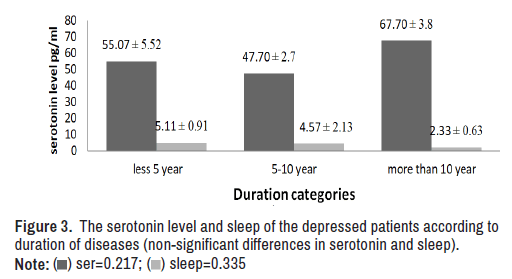
The mean differences in serotonin level according to sleep categories show non -significant differences within the depression patient groups (p=0.110) and control groups (p=0.439).
Figure 2 means differences of serotonin level in study groups according to sleep categories (non-significant differences within the patients groups and control groups).
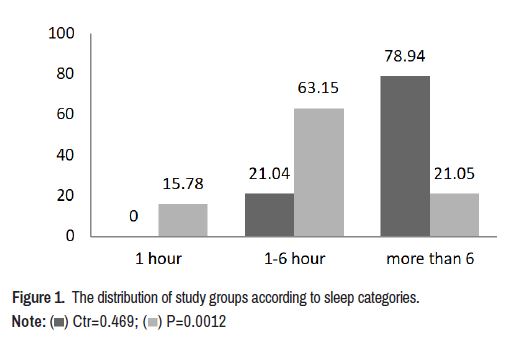
Regarding to duration three categories were depended for classified patients group less than 5 years was (47.36%), 5-10 years was (36.84%) and more than 10 years (15.78%). The serotonin level and sleep were studied according to these categories, there was non-significant differences among duration categories for serotonin level (P=0.217) and sleep (P=0.335) (Figure 3), there wasn't relation of serotonin level with sleep in different disease duration. Also serotonin decreased during the period 5-10 years while increased after 10 years of disease.
The serotonin level and sleep of the depressed patients is according to duration of diseases (non-significant differences in serotonin and sleep) (Figure 3). Sleep is a critical aspect of the pathophysiology and treatment of depression, the sleep disturbance was observed in the current study in significant decrement in patients, the disrupted of sleep times and architecture have been proved in patients with different mood disorders like depression and bipolar [12-14], others pointed that there was disturbance in quantity and quality of sleep and it has been found to be associated with neuropsychiatric disorders like schizophrenia and manic psychosis in addition to major depression that it much more typical and more pronounced [15].
In patients serotonin level was decreased with increased sleep time in current study while in control the serotonin increased with sleep time, studies refer to the role of serotonin in the emotion response but its role in wakefulness-sleep cycle didn’t completely understand [10,11], a study conducted by Elmenhorst et al., found evidence of increased levels of serotonin 2A receptor (5-HT2AR) availability in the human brain after one night of sleep deprivation, the present study found that depression patients with short sleep time have high serotonin level, this deal with Bjorvatn et al., who found by eliminating sleep, there may be a net increase in serotonergic neurotransmission during the sleep deprivation period [16,17]. Nevertheless, some investigations proposed that the serotonin production during waking may start a cascade of genomic events in some hypnogogic neurons sited in the periotic area. Thus, when serotonin is released during waking, it leads to a homeostatic regulation of slow-wave sleep [18]. Belong to duration period sleep was lower and serotonin increased when the depression period more than 10 years and decreased in the period 5-10 years, as mentioned above the relation of serotonin with the sleep still under investigations, other factors may involve in this relation like lifestyle, depression medication strategies, genome expression and some gene variations which may be affected [19,20], the relation of serotonin and depression has been studied, but the relation to depression period still under research, however present findings need more investigations to understand the relation sleep with serotonin in Iraqi patients with depression disorders. Present study concluded that serotonin affected by sleep in depression and didn’t effect by duration of disease, sleep decreased with duration increment.
Conclusion
The Present study concluded that serotonin may have affected in sleep in depression but didn’t affect by duration of disease, the results show non-significant serotonin level (P=0.566) and sleep show a significant decrement in patients than control (p=0.000), significant differences among sleep categories distribution (p=0.0012). Sleep period decrease with duration increment in depression disorder patients, there were other factors should be studied like lifestyle, nutrition, medications and some genes polymorphisms.
References
- Ford, Daniel E and Douglas B Kamerow. “Epidemiologic Study of Sleep Disturbances and Psychiatric Disorders: An Opportunity for Prevention?.” Jama 262 (1989): 1479-1484.
[Crossref] [Google scholar] [Pubmed]
- Breslau, Naomi, Thomas Roth, Leon Rosenthal and Patricia Andreski. “Sleep Disturbance and Psychiatric Disorders: A Longitudinal Epidemiological Study of Young Adults.” Biol Psychiatry 39 (1996): 411-418.
[Crossref] [Google scholar] [Pubmed]
- Chang, Patricia P, Daniel E Ford, Lucy A Mead and Lisa Cooper-Patrick, et al. “Insomnia in Young Men and Subsequent Depression: The Johns Hopkins Precursors Study.” Am J Epidem 146 (1997): 105-114.
[Crossref] [Google scholar] [Pubmed]
- Koren, Danny, Isaac Arnon, Peretz Lavie and Ehud Klein. “Sleep Complaints as Early Predictors of Posttraumatic Stress Disorder: A 1-year Prospective Study of Injured Survivors of Motor Vehicle accidents." Am J Psy 159 (2002): 855-857.
[Crossref] [Google scholar] [Pubmed]
- Neckelmann, Dag, Arnstein Mykletun and Alv A. Dahl. “Chronic Insomnia as a Risk Factor for Developing Anxiety and Depression.” Sleep 30 (2007): 873-880.
[Crossref] [Google scholar] [Pubmed]
- Buysse, Daniel J, Jules Angst, Alex Gamma and Vladeta Ajdacic, et al. “Prevalence, Course, and Comorbidity of Insomnia and Depression in Young Adults.” Sleep 31 (2008): 473-480.
- Riemann, Dieter and Ulrich Voderholzer. “Primary Insomnia: A Risk Factor to Develop Depression?.” J Affective Dis 76 (2003): 255-259.
[Crossref] [Google scholar] [Pubmed]
- Taylor, Daniel J. “Insomnia and Depression.” Sleep 31 (2008): 447.
[Crossref] [Google scholar] [Pubmed]
- Jacobs, BARRY L and Efrain C Azmitia. “Structure and Function of the Brain Serotonin System.” Physiol Rev 72 (1992): 165-229.
[Crossref] [Google scholar] [Pubmed]
- Albert, Paul R and Chawki Benkelfat. “The Neurobiology of Depression—Revisiting the Serotonin Hypothesis. II. Genetic, Epigenetic and Clinical Studies.” Philos Trans R Soc Lond B Biol Sci 368 (2013): 20120535.
[Crossref] [Google scholar] [Pubmed]
- Albert, Paul R, Chawki Benkelfat and Laurent Descarries. “The Neurobiology of Depression—Revisiting the Serotonin Hypothesis. I. Cellular and Molecular Mechanisms.” Philos Trans R Soc Lond B Biol Sci 367 (2012): 2378-2381.
[Crossref] [Google scholar] [Pubmed]
- Tsuno N, Besset A and Ritchie K. “Sleep and Depression.” J Clin Psychiatry 66 (2005):1254–1269.
- Breslau, Naomi, Thomas Roth, Leon Rosenthal and Patricia Andreski. “Sleep Disturbance and Psychiatric Disorders: A Longitudinal Epidemiological Study of Young Adults.” Biological Psychiatry 39 (1996): 411-418.
[Crossref] [Google scholar] [Pubmed]
- Ford, Daniel E, and Lisa Cooper-Patrick. “Sleep Disturbances and Mood Disorders: An Epidemiologic Perspective.” Depression Anxiety 14 (2001): 3-6.
[Crossref] [Google scholar] [Pubmed]
- Palagini, Laura, Chiara Baglioni, Antonio Ciapparelli and Angelo Gemignani, et al. “REM Sleep Dysregulation in Depression: State of the Art.” Sleep Med Rev 17 (2013): 377-390.
[Crossref] [Google scholar] [Pubmed]
- Elmenhorst, David, Tina Kroll, Andreas Matusch and Andreas Bauer. “Sleep Deprivation Increases Cerebral Serotonin 2A Receptor Binding in Humans.” Sleep 35 (2012): 1615-1623.
[Crossref] [Google scholar] [Pubmed]
- Bjorvatn, BJ. Grønli, F. Hamre and E Sørensen, et al. “Effects of Sleep Deprivation on Extracellular Serotonin in Hippocampus and Frontal Cortex of the Rat.” Neuroscience 113 (2002): 323-330.
[Crossref] [Google scholar] [Pubmed]
- Jouvet, Michel. “Sleep and Serotonin: An Unfinished Story.” Neuropsychopharmacology 21 (1999): 24S-27S.
[Crossref] [Google scholar] [Pubmed]
- Kadhum, Aamal Muhsen, Eman Salih Abd and Ruaa Amer Taleb, et al. “Genetic Polymorphisms of Mitochondrial Genes (ND1, ATP6c) in Depression Patients.” NeuroQuantology 19 (2021): 128-133.
- Kadhum, Aamal Muhsen, Bayader M Abd Al-Kadim, Thanaa Chasib Kareem and Ali Ahmed Nayyef, et al. “Associations of Tumor Necrosis Factor-[alpha] G-308A (rs1800629) Gene Polymorphisms with Major Depressive Disorder.” NeuroQuantology 19 (2021): 133-137.
Citation: Thanoon, Allaa Hatim, Mohammed Abed Jawad, Mohammed Haider Hamad and Mohammed Shakir Atiyah, et al. “The Effect of Sleep in Serotonin Level for Different Duration Periods of Depression Disorders.” Clin Schizophr Relat Psychoses 16S (2022). Doi: 10.3371/CSRP. TAMJ.121022.
Copyright: © 2022 Thanoon AH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.







 ) Ctr=0.469; (
) Ctr=0.469; ( ) P=0.0012
) P=0.0012