Review Article - Clinical Schizophrenia & Related Psychoses ( 2021) Volume 0, Issue 0
2Department of Psychology, The Sixth Medical Center, Chinese People's Liberation Army General Hospital, Beijing, China
3Department of Infection Control, The Sixth Medical Center, Chinese People's Liberation Army General Hospital, Beijing, China
Yanfei He, Health Management Center, The Sixth Medical Center, Chinese People's Liberation Army General Hospital, Beijing, China, Email: heyanfeilc@163.com
Received: 15-Mar-2021 Accepted Date: Mar 29, 2021 ; Published: 05-Apr-2021, DOI: 10.3371/CSRP.HYYR.032521
Abstract
Since December 2019, the havoc caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has increased exponentially in a short period of time. As the COVID-19 pandemic is raging around the world, scientists are trying to reveal its mysteriousness. Although COVID-19 is predominantly a respiratory disease, the most common symptoms are fever, dry cough, and fatigue, but extrapulmonary manifestations are increasingly recognized. Recent studies have shown that there is a strong genetic correlation between one or more psychiatric disorders and the occurrence of SARS-CoV-2 infection. Historical epidemiological perspectives and recent neurobiological evidence link infection and psychosis. What is the relationship between COVID-19 and psychiatric disorders? In this article, we will review the correlation between COVID-19 and psychoses, the possible reasons, and the possible pathophysiological mechanisms. The purpose of this review is to provide a reference for clinicians to make correct judgment and treatment when facing patients with COVID-19 and/or psychiatric disorders.
Keywords
Psychiatric disorder • COVID-19 • SARS-CoV-2 • Psychiatry • Psychosis • Neuropsychiatry • Schizophrenia
Introduction
COVID-19 pandemic is not only a great impact on almost all aspects of personal life and organization in the world but also an important source of psychological stress [1,2]. The unpredictability and uncertainty of the COVID-19 epidemic, related blockades, physical distances, and other containment strategies, as well as the resulting economic collapse, may increase the risk of psychiatric disorders [3,4]. Recently, there have been more and more studies on the relationship between COVID-19 and psychoses [5,6]. However, there is little information to date on a comprehensive review of the subject. In this review, we collect evidence of the associations between COVID-19 and psychoses, the possible reasons, and mechanisms. Our purpose is to remind clinicians that when facing patients suspected of COVID-19, they should consider that COVID-19 may be complicated with psychiatric disorders, to avoid misdiagnosis of COVID-19. At the same time, early diagnosis and treatment of psychoses in patients with COVID-19 can prevent further deterioration of late neuropsychiatric complications.
Clinical Implications
The COVID-19 epidemic has caused disasters on a global scale and has become an important source of psychological stress for people around the world, which may increase the risk of psychiatric disorders. There are more and more studies on the relationship between COVID-19 and psychoses and show that there must be some associations between them. But what is the correlation between COVID-19 and psychiatric disorders? What are the reasons? What are the possible pathophysiological mechanisms? This review collects the evidence of the associations between COVID-19 and psychoses, illustrates the etiology of the psychiatric consequences of the COVID-19 pandemic may be multifactorial, including brain infection, direct effects of cerebrovascular disease in a hypercoagulable state, response to pandemic-related stress (such as health intervention, social isolation or stigma), drug use (such as corticosteroids or antiviral drugs), and vertical transmission. The possible pathophysiological mechanisms include direct viral infection, inflammatory reaction, autoimmunity, hypoxia, and hypercoagulable state. Long-term follow-up and prospective studies are necessary to determine the real effect of SARS-CoV-2 on psychopathology.
Literature Review
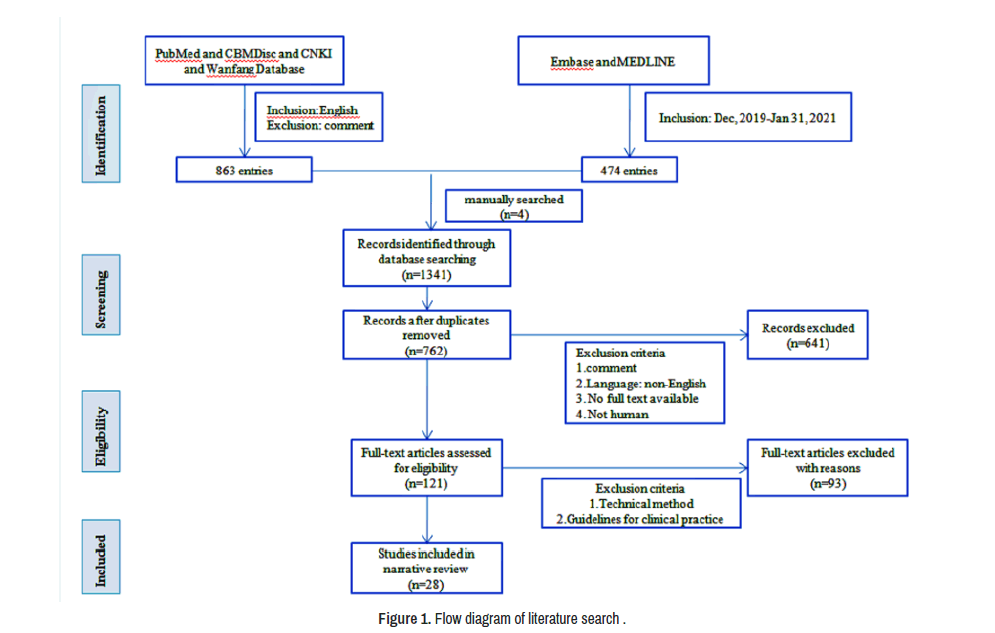
Literature published in English from December 2019 to January 31, 2021, was included in the search. We searched Pubmed, Embase, Medline, CBMDisc, CNKI, and Wanfang Database with the following search terms "COVID-19", "SARS-CoV-2", "Neurology", "Psychomotor disorders", "Mental health", "Neurocognitive disorders", "Neuropsychiatry", "Delirium", "Schizophrenia", "Hallucinations", "Delusions" and "Psychosis". We obtained a total of 1337 publications, adding 4 manually searched papers to a total of 1341. We excluded repetitive publications. News articles, reports, and other grey literature were included if they contained quantifiable evidence. After reading full texts and synthesizing relevant evidence, literature was organized thematically. Themes were discussed and decided upon by all three authors, and 28 were included in the narrative review. See (Figure 1) for a visual representation of inclusion and exclusion.
The correlation between COVID-19 and psychiatric disorders
The arrival of a pandemic may become the main trigger for the beginning or aggravation of some harmful psychological characteristics, which may lead to behavioral/mental symptoms of clinical concern, which in turn will increase individual susceptibility to COVID-19 and aggravate the severity of COVID-19. Many studies have shown that COVID-19 is closely related to psychoses recently.
COVID-19 may increase the incidence of psychiatric disorders and aggravate the severity of the original psychiatric disorders.
COVID-19 is a potentially fatal disease and a major source of stress for COVID-19 patients. During the pandemic, isolation, social distance, personal income instability caused by a sharp rise in unemployment, a shortage of social life resources, limited hospital resources, and barriers to access to health care caused by stigma, these are the main problems that emerged during the COVID-19 pandemic, all of them may lead to a negative impact on mental health [7-9], and people with mental disorders may be more vulnerable to these negative effects [10-13]. An observational study showed that the number of cases of schizophrenia increased by 25% in January 2020 compared with previous years, which was attributed to the psychosocial stress and physical distance measures related to the COVID-19 outbreaks [14]. The review by Brown, et al. postulated that there was a correlation between the high risk of psychiatric disorders and the psychosocial stress caused by the COVID-19 pandemic. The incidence of psychoses in confirmed COVID-19 patients is between 0.9% and 4% [15]. Zheng, et al. noted a high prevalence of psychiatric disorders among survivors of the COVID-19 epidemic [16]. A research showed that patients with Obsessive-Compulsive Disorder (OCD) quarantined during the COVID-19 outbreak had higher obsessions and compulsions symptoms than before the outbreak [17].
National quarantine regulations during outbreaks make it more difficult and impractical to regularly go to outpatient clinics for evaluation and obtain prescription psychotropic substances, which can also increase the recurrence or deterioration of their pre-existing signs and symptoms [18]. Also, COVID-19 infection per se and severe side effects of antiviral treatment may also aggravate some symptoms of psychiatric patients [19-21]. Individuals who suffer from mental health issues may be more especially vulnerable to the emotional response of the COVID-19 epidemic, resulting in worsening symptoms of pre-existing psychiatric disorders and/or an increased recurrence rate, because compared with the general population, they are highly sensitive to stress, such as alcohol substance use [22], eating disorders [23]. Symptoms of anxiety and depression, as well as high-stress levels, were reported after the outbreak [24].
Patients with pre-existing psychiatric disorders are more susceptible to COVID-19 and can aggravate the severity of COVID-19
Pre-existing psychiatric disorders may also change the individual susceptibility to COVID-19 [25]. When epidemics occur, people with psychiatric disorders are generally more vulnerable to infection [26]. Emerging evidence suggests that there is a strong genetic link between at least one psychiatric diagnosis and the occurrence of infection, which provides additional support for this thought. Individuals with psychiatric disorders have a higher risk of developing COVID-19, especially the hospitalization and mortality associated with COVID-19. A variety of factors may contribute to a higher risk of SARS-CoV-2 infection and worse outcomes in people with psychiatric disorders [27]. First, psychiatric disorders may increase the risk of infections [28,29]. Possible explanations include cognitive impairment, lack of risk awareness, reduction in personal protection measures (such as hand washing, social distance, or isolation), and restrictions in psychiatric wards. Secondly, people with pre-existing mental disorders may face more barriers in accessing timely medical services after being infected with COVID-19 [30], because of discrimination related to psychoses in the health care environment and their knowledge, skills, and access barriers to using telemedicine. Third, the coexistence of psychiatric disorders and COVID-19 will make the treatment more challenging and maybe less effective [31]. For example, people with known OCD may frequently self-monitor their temperature to check for fever, or they may try to swallow saliva several times to check for throat pain as a symptom of COVID-19. Hand-washing is an important preventive measure for COVID-19 transmission, which further aggravates the suffering of patients with known washer OCD. Finally, individuals with severe psychiatric disorders are more likely to suffer from co-existing diseases associated with a higher risk for severe COVID-19. Studies have shown that co-existing diseases (such as cancer, cardiovascular disease, obesity, type 2 diabetes) contributed to higher SARS-CoV-2 infection risk in patients with recent psychosis [13,32]. Patients with both COVID-19 and recently diagnosed psychiatric disorders have an increased risk of death [33].
Possible reasons
The etiology of the psychiatric consequences of the current COVID-19 pandemic may be multifactorial, including brain infection, direct effects of cerebrovascular disease in a hypercoagulable state, response to pandemic-related stress (such as health intervention, social isolation, or stigma) [34], drug use (such as corticosteroids or antiviral drugs), and vertical transmission.
Reactive response to pandemic-related stress: The social distance and other public health interventions to curb the spread of COVID-19 may have an immediate and long-term impact on people with psychosis or people at risk of psychiatric disorder [15]. During the pandemic, almost every country has developed public health strategies to curb the spread of COVID-19, including quarantine of people who may be exposed to the virus and requiring a physical distance from the general population [35]. The incidence of depression and anxiety in people who implement social distance may be affected [36]. Despite telecommunications tools exist, distrust or unfamiliarity with technology may be additional pressure for people with mental disorders who use such tools. The COVID-19 pandemic has caused a considerable increase in unemployment rates, restricting individuals with psychiatric disorders from having a steady income, limiting their access to food, permanent housing, and medicine [37]. Shortages of resources that patients rely on, such as transportation, groceries, and services from public buildings, further disrupt daily life. In addition, there are the impacts of reduced physical activity, dietary changes, and reduced sunlight exposure [38]. A study indicated that self-isolation was related to the increased C-Reactive Protein (CRP) level [39]. Busch, et al. noted that individuals with greater stress were associated with higher inflammation levels [40]. These results provide a basis for the conclusion of this study: self-isolation is a special form of inflammation. This can arise through psychosocial stressors irrespective of infection, for example, fear, isolation, bereavement, homelessness, broken relationships (divorce/separation), unemployment and financial difficulties, domestic violence, and deteriorating physical health. Given their susceptibility to social health determinants, all of these may have a particular effect on psychiatric patients [24,41-43]. Similarly, the direction of this effect is unclear, as pandemics have the potential to strengthen social inequalities, which in turn may lead to a risk of exceeding the consequences of the infection itself, further complicating the interaction between COVID-19 and psychiatric disorders.
SARS-CoV-2 infection: The effect of SARS-CoV-2 infection on the brain is associated with the excessive physiological and psychological stress of stimulating the hypothalamic-pituitary-adrenal axis, which further aggravates neuroinflammatory status. The duration and frequency of exposure to stressors impact neuroinflammation, which can be exacerbated by repeated or prolonged exposure to strong stressors [44]. Long-term stress can enhance inflammatory response by releasing several pro-inflammatory cytokines. Neuroinflammation is an important aetiological factor for many neuropsychiatric and neurocognitive diseases, including neurodegenerative disorders, depression, psychosis, autism, drug abuse, and sleep disorders [45-50]. A study on neuropsychiatric consequences of SARS conducted 30-50 months after infection showed an incidence of post-traumatic stress disorder (PTSD) was 40%, depression was 36.4%, OCD was 15.6%, and with the same incidence of anxiety disorders [51]. Given this evidence, the sequelae of long-term post-SARS-CoV-2 psychiatric disorders are noteworthy. A recent study indicated the neuroinvasive nature of the virus and its possible route of transmission to the central nervous system by transmission electron microscopy of the brain tissue of a 74-year-old male patient with COVID-19 [52]. It has clearly demonstrated that there are 80 to 110 nm viral particles in the vesicles of the frontal lobe and endothelial cells. Besides, the blebbing of viral particles in or out of the endothelial wall indicates the viral entry or exit across the brain micro vascular endothelial cells into the nervous system.
Corticosteroids and/or chloroquine and other antiviral drugs: Corticosteroids usually induce psychiatric syndrome, including depression, mania, psychosis, and delirium, which is often referred to as 'steroid psychosis' and is considered to be a representative exogenous psychosis [53, 54]. However, steroid psychosis is not a specific clinical entity but consists of heterogeneous syndromes with significantly different pathophysiological mechanisms. Psychiatric symptoms may also be secondary to side effects of drugs such as interferon and oseltamivir used to treat COVID-19 [19,20]. A pharmacovigilance study reported obviously neuropsychiatric side effects associated with chloroquine exposure, such as amnesia, hallucinations, depression, delirium, and loss of consciousness [21]. The severity of COVID-19 symptoms and higher doses of corticosteroids were significantly related to an increased risk of experiencing psychiatric symptoms. Chloroquine may affect the dopaminergic system in the brain by changing dopamine levels, which in most cases is a high dopaminergic response. There is a substantial meta-analysis of evidence that proinflammatory cytokines are elevated in patients with primary psychosis. In fact, drugs targeting specific cytokines can cause psychosis [55-58]. High-dose steroid use has also been identified as a probable risk factor for psychosis, according to a case-control study in China [59].
Encephalopathy and encephalitis: Encephalopathy in COVID-19 may be the direct viral effect of neural invasion, an immune-mediated pathology induced by the virus, an indirect immunopathology caused by blood-brain barrier dysfunction, or a combination of all three. The virus enters the central nervous system by infecting endothelial cells of the blood-brain-barrier, epithelial cells of the blood-cerebrospinal fluid barrier in the choroid plexus, or by inflammatory cells [60,61]. More importantly, the virus can reach the central nervous system by retrograde axonal transport. Retrograde axonal transport may be carried out through olfactory, respiratory, and enteric nervous system networks. After infecting the nasal cells, the virus can directly invade the brain, possibly through the olfactory bulbs, and rapidly spread to specific brain areas such as the thalamus and brainstem, triggering inflammation and demyelination [62]. SARS-CoV-2 has been detected in the cerebrospinal fluid of many patients with various psychiatric symptoms [63,64], it has provided undeniable evidence that SARS-CoV-2 can invade the nervous system. Two studies reported that 20% of patients had a complication of hypoxic encephalopathy following COVID-19, and patients who died were more likely to develop hypoxic encephalopathy than those who survived [65,66].
Vertical transmission: Several cross-sectional studies have shown that maternal stress, health anxiety, and social behavior interaction have changed significantly [67,68]. The current COVID-19 pandemic may affect the fetal neurodevelopment of pregnant women during the pandemic by activating the immune system, directly due to maternal immune activation during infection, and indirectly due to inflammation exposed to maternal pressure during pregnancy. Inflammation is the common mediator of these two mechanisms. Isolation and limited movement may lead to a lack of social support from friends, relatives, and partners for pregnant women. Financial hardship, remote work, potentially violence from intimate partners, fewer pre-and post-natal appointments, and changes related to breastfeeding recommendations, which are a huge source of stress for perinatal women and their babies and can have short-and long-term harmful effects on pregnant women and babies [69,70]. At the same time, studies have shown that vulnerable pregnant women are also high-risk groups with higher stress due to fear of infection or transmission of SARS-CoV-2 [36,71]. SARSCoV- 2 infection potentially triggers the maternal immune system to release a series of cytokines and chemokines (such as Tumor Necrosis Factor-Alpha, -alpha [TNF-α], and other immune changes that may be transmitted to the foetus. Besides, critically ill pregnant women caused by COVID-19 are at risk of placental hypoxia, damaging foetal oxygen supply, which may cause growth restriction and brain development stagnation. Studies have shown that maternal immune activation can lead to psychiatric disorders through multiple potential trajectories, thus making the offspring vulnerable to the environmental risks for psychosis [72]. A recent review summarizes the mechanisms, including the effects associated with each trimester, the direct impacts of viruses reaching the foetus, and the effects of maternal and foetal immune activation [73]. IgG antibodies and cytokines may passively cross the placental barrier, while IgM usually does not due to its larger molecular structure, suggesting that antibodies may be produced by the infant to cope with intrauterine SARS-CoV-2 infection. One area of psychiatric research that may provide a precedent for the longitudinal effect of COVID-19 is the relationship between intrauterine events and neurodevelopment of offspring [72,74]. Therefore, it will be important to closely monitor the outcomes of children whose mothers infected prior to, and during, pregnancy.
Clinical Manifestations of Psychosis
Psychosis is a state of serious disconnection between personal experience and reality or loss of self-boundaries. It is mainly manifested in the existence of hallucinations and delusions. Psychosis is a hallmark or defined symptom of schizophrenia spectrum and other mental disorders, and it is related to the characteristics of other mental and behavioral disorders. The systemic inflammation and neuroinflammatory changes are related to the massive increased brain pro-inflammatory molecules, glial reactivity, neurochemical landscape alternation, and pathological remodeling of neural networks. These organic changes are accompanied by environmental stress and promote the pathological disorder of neuropsychiatry.
Psychosis can be considered to be a set of symptoms, and there are a variety of manifestations in COVID-19 patients, ranging from insomnia and anxiety to psychiatric symptoms and aggressive behavior. This pattern of psychiatric symptoms is similar to those of patients infected with SARS in previous studies, ranging from mild mental problems (such as anger, anxiety, and depressive reactions) to severe psychotic problems such as hallucinations and mania [75,76]. A study shows that the most common mental symptoms of COVID-19 patients on admission are insomnia, followed by aggressive behavior, delusions, and severe anxiety [77]. Besides, it is characterized by depression [78], substance-related and addiction disorders [79], eating disorders, schizophrenia [15], reactive psychosis, panic attacks, OCD, post-traumatic stress disorder, agoraphobia, and other psychiatric disorders.
Possible Pathophysiological Mechanisms
The postulated common pathophysiologic mechanisms by SARSCoV- 2 include direct viral infection, inflammatory response, autoimmunity, hypoxia, and hypercoagulable state.
SARS-CoV-2 structure and ACE2 receptor
COVID-19 pneumonia is caused by SARS-CoV-2 [80], as the seventh known coronavirus that can infect humans (humans coronavirus, H-CoV). The first six coronaviruses that can cause severe diseases in humans include Middle East Respiratory Syndrome (MERS)-CoV, HCoV-HKU1, HCoVOC43, HCoV-NL63, SARS-CoV, and HCoV-229E [81]. The SARS-CoV-2 virion is approximate with a size of 70-100 nm [82], its genome encodes four main structural proteins: Spike (S), Envelope (E), Membrane (M), and Nucleocapsid (N). Recent studies have shown that some coronaviruses do not require all four proteins to become infectious virions [83].
ACE2 receptors are recognized as the SARS-CoV-2 receptor so far, which exist in a variety of human tissues, including type I and II alveolar epithelial cells, vascular endothelial cells, heart, liver, gastrointestinal tract [84], as well as kidneys and testicles [85]. It also presents at the cellular level of the central nervous system, such as the spinal cord, cortex, hippocampus, and cerebellum [86,87]. S and E proteins play a critical role in aiding SARS-CoV-2 S proteins to interact with ACE2 receptors expressed in capillary endothelium [88].
Direct infection
The first step of SARS-CoV-2 infection is the recognition of host cell surface receptors. This step is mediated by the viral S protein, which recognizes the human receptor Angiotensin-Converting Enzyme 2 (ACE2). The protein has two functional domains: The S1 domain contains the Receptor-Binding Domain (RBD), which binds to ACE2, while the S2 domain mediates the fusion of the virus and the host cellular membrane [89]. Therefore, the organ distribution of the ACE2 receptor is an important determinant of the virus infectivity and tropism. The second determinant step of the SARS-CoV-2 infection process is the activation of the S protein. This protein processing allows the complete activity of the S2 domain and the fusion of the viral and cellular membrane. The SARS-CoV-2 enters the cell following binding to the plasmalemmal ACE2 enzyme and then endocytosis [90,91]. Literature suggests the enriched presence of Angiotensin-Converting Enzyme 2 (ACE2) in the Central Nervous System (CNS) endothelial cells. Possibly the virus infects these endothelial cells in the CNS by crossing the blood-brain barrier [65,92,93]. The neuronal retrograde mode is also suggested in a few studies, in which the virus initially invades the peripheral nervous system followed by infecting the CNS [52,94], neurotropic viruses may invade neurons through virion retrograde or/and anterograde interactions with neuronal cytoskeleton proteins. After neuronal infection, the virions may be released and transneuronal spread to adjacent or presynaptic neurons [95,96].
Inflammatory reaction
A growing body of evidence suggests that psychiatric disorders of COVID-19 patients may be associated with the level of inflammatory markers. It is well known that COVID-19 can cause increased levels of serum inflammatory markers by activating an immune response [97]. Meta-analysis data confirmed that there was a significant increase in proinflammatory molecules in patients with post-traumatic stress disorder, including IL-6, TNF-α, and IL-1β [98,99]. However, the significance of the acute inflammatory state in the occurrence and development of neuropsychiatric sequela is unclear, which stems not only from the severity of systemic inflammation and the invasion of the brain by the virus but also from the severity of stress caused by unexpected pandemics [100]. The alterations of GABA-ergic and dopaminergic regulation in the corticobasal ganglia-thalamocortical circuit are related to its pathogenesis [101]. Exposure to pro-inflammatory cytokines is associated with altered GABAergic transmission in the basal ganglia. Other pro-inflammatory mediators such as interferon-alpha are considered to be associated with a hypodopaminergic state in the basal ganglia, which is considered to be a potential inducing factor to psychiatric disorders. Also, the hematological high inflammatory state of COVID-19 patients increases the blood-brain barrier permeability, destroys brain cells, and becomes a promoting factor for the occurrence of psychoses. A recent report on a case of psychosis patient with COVID-19 further implicates that the hyper-inflammatory state is related to the pathogenesis of these neuropsychiatric complications of severe COVID-19 [102]. Besides, inflammation is an example of a common biological factor that contributes to various psychiatric disorders and COVID-19 pathology. It is reported that inflammation plays a role in the pathogenesis of schizophrenia, depression, and bipolar disorder, as well as in the systemic manifestations of SARS-CoV-2 infection [103-106].
Autoimmunity
When an individual with immune function is infected with SARS-CoV-2, he may experience excessive systemic immune responses and even die of acute respiratory distress syndrome and septic shock [107]. This mechanism is called immunopathogenicity, in which the virus stimulates immunity and causes the immune system to attack itself [108]. The excessive activation of the immune system caused by SARS-CoV-2 infection leads to massive accumulation and exudation of inflammatory substances, which is known as 'cytokine storm'. Cytokine storm may cause a sharp increase of monocytes, interferons, interleukins, macrophage inflammatory proteins, and tumor necrosis factors, leading to hyper-inflammation. This systemic inflammation causes severe encephalopathy, which can lead to symptoms of psychiatric disorders. A high level of IL-1β. has been observed in COVID-19 patients, and other immune mediators including IL-2, IL-6, IL-7, IL-10 [109], and Granulocyte-Colony Stimulating Factor (G-SCF), which have strong pro-inflammatory effects and can cause neuroinflammation and brain dysfunction [110].
Hypoxia
COVID-19 patients often have hypoxemia caused by respiratory dysfunction [111,112], among which severe patients are characterized by acute respiratory distress syndrome [113]. When the bodily oxygen content changes, the brain is the first organ to be affected [114], resulting in a series of pathophysiological changes. Hypoxia can dilate intracranial blood vessels, increase intracranial blood flow, cerebral capillary pressure, tissue fluid production, brain free radicals, membrane lipid peroxidation, and endogenous inhibitors, which may affect cell energy metabolism [115,116]. The increased lactic acid and oxygen free radicals and lipid peroxides produced by anaerobic glycolysis in the brain, and the weakened antioxidant system lead to blood-brain barrier dysfunction [117]. Metabolic acidosis due to hypoxia increases cerebral vasospasm and permeability, resulting in interstitial brain edema and intracranial hypertension [118], which can lead to a series of injuries, culminating in neuronal and astroglial necrosis, apoptosis, and neurocognitive deficits [119].
Hypercoagulable state
Clinical studies showed that the elevated D-dimer [120], the prolonged prothrombin time with unchanged Activated Partial Thromboplastin Time (APTT), and increased fibrinogen are commonly observed in patients with COVID-19, and the blood was in a state of hypercoagulability. One possible explanation for the increased blood coagulability is that a decreased blood oxygen activates increased the levels of inflammatory cytokines, catecholamine, plasma tissue factors [121], and platelet aggregation, which change capillary blood flow because of increased sympathetic activity and broader micro-endothelial damage, leading to increased blood coagulation [122], and capillary microthrombosis [123], which may cause ischemic damages of small vessels in the brain, leading to psychoses.
Prospects for the Future
In the long term, as symptoms and potential effects of COVID-19 continue to manifest, patients may be left with long-term neurological and/ or psychiatric disorders on a global scale [124,125]. The role of intrauterine infection in the neurodevelopment of offspring born during this pandemic may not become apparent for many years for both infected and noninfected mothers. Notably, knowledge of the long-term psychiatric effects of COVID-19 on surviving patients is almost absent. The psychiatric sequelae of COVID-19 represent a serious clinical challenge, which has to be considered in complex screening, treatment, and follow-up in the future. It is necessary to conduct a long-term follow-up and a prospective study on the direct biological impact of COVID-19 on psychoses, in order to more accurately describe the incidence of psychoses related to SARSCoV- 2 during and after infection, as well as the real effect and potential pathogenesis of SARS-CoV-2 on psychopathology.
Limitations
This review has several limitations. First, most of the current papers on clinical features were designed retrospectively, which may introduce potential biases. Second, the symptoms associated with psychoses came from limited sample size observations and case studies, some of which were not classical psychiatric manifestations, and the psychiatric participation may contribute partially to these symptoms, and an overall analysis may exaggerate its role in COVID-19. Third, many involved studies have not yet been published, which may affect the results. The potential mechanism underlying psychiatric disorders in COVID-19 will be updated along with new evidence.
Conclusion
The COVID-19 pandemic poses a long-lasting challenge, which not only impacts the cardiopulmonary system but links systemic infection to psychiatric disorders. When doctors find the symptoms of psychoses in COVID-19 patients, they should always consider differential diagnosis to avoid delay or misdiagnosis. Long-term follow-up is necessary to determine the future incidence of psychiatric disorders after SARS-COV-2 infection, and prospective studies should be conducted to find out the real impact of COVID-19 on psychopathology, and finally overcome the epidemic of COVID-19.
Funding and Financial Disclosure
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interests
The authors report no declarations of interest.
Acknowledgment
None.
References
- Cucinotta, Domenico and Maurizio Vanelli. “WHO Declares COVID-19 a Pandemic.” Acta Biomed 91 (2020):157-160.
- Taubman-Ben-Ari, Orit, Miriam Chasson, Salam Abu Sharkiam and Efrat Weiss. “Distress and Anxiety Associated with COVID-19 Among Jewish And Arab Pregnant Women In Israel.” J Reprod Infant Psychol 38 (2020):340-348.
- Rajkumar, Ravi Philip. “COVID-19 and Mental Health: A Review Of The Existing Literature.” Asian J Psychiatr 52 (2020):102066.
- Gupta, Aakriti ,Mahesh V. Madhavan, Kartik Sehgal and Nandini Nair, et al. “Extrapulmonary Manifestations of COVID-19.” Nat Med 26(2020):1017-1032.
- Nalleballe, Krishna, Sanjeeva Reddy Onteddu, Rohan Sharma and Vasuki Dandu, et al. “Spectrum of Neuropsychiatric Manifestations in COVID-19.” Brain Behav Immun 88 (2020): 71-74.
- Varatharaj, Aravinthan, Naomi Thomas, Mark A Ellul and Nicholas WS Davies, et al. “Neurological and Neuropsychiatric Complications of COVID-19 in 153 Patients: A UK-Wide Surveillance Study.”Lancet Psychiatry 7(2020):875-882
- Richardson, Safiya, Jamie S Hirsch, Mangala Narasimhan and James M Crawford, et al. “Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized with COVID-19 in the New York City Area.”JAMA 323 (2020):2052-2059.
- Myers, Laura C, Stephen M Parodi, Gabriel J Escobar and Vincent X Liu. “Characteristics of Hospitalized Adults with COVID-19 in an Integrated Health Care System in California.” JAMA 323 (2020): 2195-2198.
- Zhou, Fei, Ting Yu, Ronghui Du and Guohui Fan, et al. “Clinical Course and Risk Factors for Mortality of Adult in Patients with COVID-19 in Wuhan, China: A Retrospective Cohort Study.” Lancet 395 (2020):1054-1062.
- Ghebreyesus, Tedros Adhanom. “Addressing Mental Health Needs: An Integral Part of COVID‐19 Response.” World Psychiatry 19 (2020):129-130.
- Li, Junfeng, Zhiyun Yang, Hui Qiu and Yu Wang, et al. “Anxiety and Depression Among General Population in China at the Peak of the COVID‐19 Epidemic.” World Psychiatry 19 (2020):249-250.
- Yao, Hao, Jian-Hua Chen and Yi-Feng Xu. “Patients with Mental Health Disorders in the COVID-19 Epidemic.” Lancet Psychiatry 7(2020):e21.
- Shinn, Ann K and Mark Viron. “Perspectives on the COVID-19 Pandemic and Individuals with Serious Mental Illness.” J Clin Psychiatry 81 (2020):13412.
- Hu, W, L Su, J Qiao and J Zhu. “COVID-19 Outbreak Increased Risk of Schizophrenia in Aged Adults.” PsyChinaXiv (2020).
- Brown, Ellie, Richard Gray, Samantha Lo Monaco and Brian O'Donoghue, et al. “The Potential Impact of COVID-19 on Psychosis: A Rapid Review of Contemporary Epidemic and Pandemic Research.” Schizophr Res 222 (2020):79-87.
- Zheng, Wei. “Mental Health and a Novel Coronavirus (2019-nCoV) in China.” J Affect Disord 269 (2020):201-202.
- Davide, Prestia, Pozza Andrea, Olcese Martina and Escelsior Andrea, et al. “The Impact of the COVID-19 Pandemic on Patients with OCD: Effects of Contamination Symptoms and Remission State before the Quarantine in a Preliminary Naturalistic Study.” Psychiatry Research 291(2020):113213.
- Mao, Ling, Mengdie Wang, Shanghai Chen and Quanwei He, et al. “Neurological Manifestations of Hospitalized Patients with COVID-19 in Wuhan, China: A Retrospective Case Series Study.” MedRxiv 77 (2020) 683-690.
- Russell, Clark D, Jonathan E Millar and J Kenneth Baillie. “Clinical Evidence does not Support Corticosteroid Treatment for 2019-nCoV Lung Injury.” Lancet 395 (2020): 473-475.
- Cortegiani, Andrea, Giulia Ingoglia, Mariachiara Ippolito and Antonino Giarratano, et al. “A Systematic Review on the Efficacy and Safety of Chloroquine for the Treatment of COVID-19.” J Crit Care 57 (2020):279-283.
- Sato, Kenichiro, Tatsuo Mano, Atsushi Iwata and Tatsushi Toda. “Neuropsychiatric Adverse Events of Chloroquine: A Real-World Pharmacovigilance Study Using the FDA Adverse Event Reporting System (FAERS) Database.” Bio Sci Trends 14 (2020):139-143.
- Sun, Yan, Yangyang Li, Yanping Bao and Shiqiu Meng, et al. “Brief Report: Increased Addictive Internet and Substance Use Behavior During the COVID‐19 Pandemic in China.” Am J Addict 29 (2020): 268-270.
- Castellini, Giovanni, Emanuele Cassioli, Eleonora Rossi and Matteo Innocenti, et al. “The Impact of COVID‐19 Epidemic on Eating Disorders: A Longitudinal Observation of Pre Versus Post Psychopathological Features in a Sample of Patients with Eating Disorders and a Group of Healthy Controls.” Int J Eat Disord 53 (2020):1855-1862.
- Mazza, Cristina, Eleonora Ricci, Silvia Biondi and Marco Colasanti, et al. “A Nationwide Survey of Psychological Distress Among Italian People During the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors.” Int J Environ Res Public Health 17 (2020):3165.
- Holmes, Emily A, Rory C O'Connor, V Hugh Perry and Irene Tracey, et al. “Multidisciplinary Research Priorities for the COVID-19 Pandemic: A Call for Action for Mental Health Science.” Lancet Psychiatry 7 (2020):547-560.
- Batty, GD, IJ Deary, M Luciano and DM Altschul, et al. “Psychosocial Factors and Hospitalisations for COVID-19: Prospective Cohort Study Based on a Community Sample.” Brain, Behav ISmmun 89 (2020):569-578.
- Nudel, Ron, Yunpeng Wang, Vivek Appadurai and Andrew J, et al. “A Large-Scale Genomic Investigation of Susceptibility to Infection and its Association with Mental Disorders in the Danish Population.” Transl Psychiatry 9 (2019): 283.
- Xiao, Chunfeng. “A Novel Approach of Consultation on 2019 Novel Coronavirus (COVID-19)-Related Psychological and Mental Problems: Structured Letter Therapy.” Psychiatry Investig 17 (2020):175-176.
- Hamada, Kareem and Xiaoduo Fan. “The Impact of COVID-19 on Individuals Living with Serious Mental Illness.” Schizophr Res 222 (2020) 3-5.
- Muruganandam, Partheeban, Srinivasan Neelamegam, Vikas Menon and Johndinesh Alexander, et al. “COVID-19 and Severe Mental Illness: Impact on Patients and its Relation with their Awareness about COVID-19.” Psychiatry Res 291(2020):113265.
- Asmundson, Gordon JG and Steven Taylor. “How Health Anxiety Influences Responses to Viral Outbreaks like COVID-19: What all Decision-Makers, Health Authorities, and Health Care Professionals Need to Know.” J Anxiety Disord 71 (2020):102211.
- Alessi, Janine, Giovana Berger, De Oliveira and Debora Wilke, et al. “Mental Health in the Era of COVID-19: Prevalence of Psychiatric Disorders in a Cohort of Patients with Type 1 and Type 2 Diabetes During the Social Distancing.” Diabetol & Metab Syndr 12 (2020): 1-10.
- Wang, QuanQiu, Rong Xu and Nora D Volkow. “Increased Risk of COVID‐19 Infection and Mortality in People with Mental Disorders: Analysis from Electronic Health Records in the United States.” World Psychiatry 20 (2021):124-130.
- Wasserman, Danuta, Miriam Iosue, Anika Wuestefeld and Vladimir Carli. “Adaptation of Evidence‐Based Suicide Prevention Strategies During and After the COVID‐19 Pandemic.” World psychiatry 19 (2020): 294-306.
- World Health Organization. Coronavirus Disease 2019 (COVID-19). (2020)
- Brooks, Samantha K, Rebecca K Webster, Louise E Smith and Lisa Woodland. “The Psychological Impact of Quarantine and How to Reduce it: Rapid Review of the Evidence.” Lancet 395 (2020): 912-920.
- Yancy, Clyde W. “COVID-19 and African Americans.” Jama 323 (2020):1891-1892.
- Lippi,Giuseppe, Brandon M Henry and Fabian Sanchis-Gomar. “Physical Inactivity and Cardiovascular Disease at the Time of Coronavirus Disease 2019 (COVID-19).” Eur J Prev Cardiol 27 (2020):906-908.
- Uchino, Bert N, Ryan Trettevik, Robert G Kent de Grey and Sierra Cronan, et al. “Social Support, Social Integration, and Inflammatory Cytokines: A Meta-Analysis.” Health Psychol 37 (2018):462-471.
- Busch, Evan L, Eric A Whitsel, Candyce H Kroenke and Yang C Yang. “Social Relationships, Inflammation Markers, and Breast Cancer Incidence in the Women’s Health Initiative.” Breast 39 (2018): 63-69.
- Odriozola-González, Paula, Álvaro Planchuelo-Gómez, María Jesús Irurtia and Rodrigo de Luis-García. “Psychological Effects of the COVID-19 Outbreak and Lockdown Among Students and Workers of a Spanish University.” Psychiatry Res 290 (2020):113108.
- Wang, Cuiyan, Riyu Pan, Xiaoyang Wan and Yilin Tan, et al. “A Longitudinal Study on the Mental Health of General Population During the COVID-19 Epidemic in China.” Brain Behav Immun 87 (2020):40-48.
- Anglin, Deidre M, Sandro Galea and Peter Bachman. “Going Upstream to Advance Psychosis Prevention and Improve Public Health.” JAMA Psychiatry 77 (2020):665-666.
- O'Callaghan, James P and Diane B Miller. “Neuroinflammation Disorders Exacerbated by Environmental Stressors.” Metabolism 100 (2019):153951.
- Bright, Fiona, Eryn L Werry, Carol Dobson-Stone and Olivier Piguet, et al. “Neuroinflammation in Frontotemporal Dementia.” Nat Rev Neurol 15 (2019):540-555.
- Bakunina, Nataliia, Carmine M Pariante and Patricia A Zunszain. “Immune Mechanisms Linked to Depression Via Oxidative Stress and Neuroprogression.” Immunology 144 (2015): 365-373.
- Marques, Tiago Reis, Abhishekh H Ashok, Toby Pillinger and Mattia Veronese, et al. “Neuroinflammation in Schizophrenia: Meta-Analysis of in Vivo Microglial Imaging Studies.” Psychol Med 49 (2019):2186-2196.
- Bjørklund, Geir, Khaled Saad, Salvatore Chirumbolo and Janet K Kern, et al. “Immune Dysfunction and Neuroinflammation in Autism Spectrum Disorder.” Acta Neurobiol Exp 76 (2016):257-268.
- Kohno, Milky, Jeanne Link, Laura E Dennis and Holly McCready.“Neuroinflammation in Addiction: A Review of Neuroimaging Studies and Potential Immunotherapies.” Pharmacol Biochem Behav 179 (2019):34-42.
- Nadjar, Agnes, Henna-Kaisa M Wigren and Marie-Eve Tremblay. “Roles of Microglial Phagocytosis and Inflammatory Mediators in the Pathophysiology of Sleep disorders.” Front Cell Neuro 11 (2017): 250.
- Troyer, Emily A, Jordan N Kohn and Suzi Hong. “Are we Facing a Crashing Wave of Neuropsychiatric Sequelae of COVID-19? Neuropsychiatric Symptoms and Potential Immunologic Mechanisms.” Brain Behav Immun 87 (2020):34-39.
- Paniz‐Mondolfi, Alberto, Clare Bryce, Zachary Grimes and Ronald E. Gordon, et al. “Central Nervous System Involvement by Severe Acute Respiratory Syndrome Coronavirus‐2 (SARS‐CoV‐2).” J Med Virol 92 (2020):699-702.
- Kershner, Pamela and Rebekah Wang-Cheng. “Psychiatric Side Effects of Steroid Therapy.” Psychosomatics 30 (1989):135-139
- Lewis, David A and Robert E Smith. “Steroid-Induced Psychiatric Syndromes: A Report of 14 Cases and a Review of the Literature.” J Affect Disord 5 (1983): 319-332.
- Pillinger, Toby, Emanuele F Osimo, Stefan Brugger and Valeria Mondelli, et al. “A meta-Analysis of Immune Parameters, Variability and Assessment of Modal Distribution in Psychosis and Test of the Immune Subgroup Hypothesis.” Schizophr Bull 45 (2019):1120-1133.
- Goldsmith, DR, MH Rapaport and BJ Miller. “A Meta-Analysis of Blood Cytokine Network Alterations in Psychiatric Patients: Comparisons Between Schizophrenia, Bipolar Disorder and Depression.” Mol Psychiatry 21 (2016):1696-1709.
- Miller, Brian J, Peter Buckley, Wesley Seabolt and Andrew Mellor, et al. “Meta-Analysis of Cytokine Alterations in Schizophrenia: Clinical Status and Antipsychotic Effects.” Biol Psychiatry 70 (2011): 663-671.
- Essali, Norah, David R Goldsmith, Laura Carbone and Brian J Miller. “Psychosis as an Adverse Effect of Monoclonal Antibody Immunotherapy.” Brain Behav Immun 81 (2019):646-649
- Lee, Dominic TS, YK Wing, Henry CM Leung and Joseph JY Sung, et al. “Factors Associated with Psychosis Among Patients with Severe Acute Respiratory Syndrome: A Case-Control Study.” Clin Infect Dis 39 (2004):1247-1249.
- Li, Yan‐Chao, Wan‐Zhu Bai and Tsutomu Hashikawa. “The Neuroinvasive Potential of SARS‐CoV2 May Play a Role in the Respiratory Failure of COVID‐19 Patients.” J Med Virol 92 (2020): 552-555.
- Toljan, Karlo. "Letter to the Editor Regarding the Viewpoint “Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host–Virus Interaction, and Proposed Neurotropic Mechanism”. ACS Chem Neurosci 11 (2020):1192-1194.
- Bohmwald, Karen, Nicolas Galvez, Mariana Ríos and Alexis M Kalergis. “Neurologic Alterations Due to Respiratory Virus Infections.” Front Cell Neuroscience 12 (2018): 386.
- Andriuta, Daniela, Pierre-Alexandre Roger, William Thibault and Bénédicte Toublanc, et al. “COVID-19 Encephalopathy: Detection of Antibodies Against SARS-CoV-2 in CSF.” J Neurol 267 (2020): 2810-2811.
- Virhammar, Johan, Eva Kumlien, David Fällmar and Robert Frithiof, et al. “Acute Necrotizing Encephalopathy with SARS-CoV-2 RNA Confirmed in Cerebrospinal Fluid.” Neurology (2020): 445-449.
- Solomon, Isaac H, Erica Normandin, Shamik Bhattacharyya and Shibani S Mukerji, et al. “Neuropathological Features of Covid-19.” N Eng J Med 383 (2020):989-992.
- Rockx, Barry, Thijs Kuiken, Sander Herfst and Theo Bestebroer, et al. “Comparative Pathogenesis of COVID-19, MERS, and SARS in a Nonhuman Primate Model.” Science 368 (2020): 1012-1015.
- Corbett, Gillian A, Sarah J Milne, Mark P Hehir and Stephen W Lindow, et al. “Health Anxiety and Behavioural Changes of Pregnant Women During the COVID-19 Pandemic.” Eur J Obstet Gynecol Reprod Biol 249 (2020): 96-97.
- Mappa, Ilenia, Flavia Adalgisa Distefano and Giuseppe Rizzo. “Effects of Coronavirus 19 Pandemic on Maternal Anxiety During Pregnancy: A Prospectic Observational Study.” J Perinat Med 48 (2020): 545-550.
- Burki, Talha. “The Indirect Impact of COVID-19 on Women.” Lancet Infect Dis 20 (2020): 904-905.
- Lancet, The. “The Gendered Dimensions of COVID-19.” Lancet 395 (2020):1168.
- Knight, Marian, Kathryn Bunch, Nicola Vousden and Edward Morris, et al. “Characteristics and Outcomes of Pregnant Women Admitted to Hospital with Confirmed SARS-CoV-2 Infection in UK: National Population Based Cohort Study.” BMJ 369 (2020):2107.
- Khashan, Ali S, Kathryn M Abel, Roseanne McNamee, and Marianne G Pedersen, et al. “Higher Risk of Offspring Schizophrenia Following Antenatal Maternal Exposure to Severe Adverse Life Events.” Arch Gen Psychiatry 65 (2008):146-152.
- Yockey, Laura J, Carolina Lucas and Akiko Iwasaki. “Contributions of Maternal and Fetal Antiviral Immunity in Congenital Disease.” Science 368 (2020):608-612.
- Brown, Alan S. “Epidemiologic Studies of Exposure to Prenatal Infection and Risk of Schizophrenia and Autism.” Dev Neurobiol 72 (2012):1272-1276.
- Lam, Marco Ho-Bun, Yun-Kwok Wing, Mandy Wai-Man Yu and Chi-Ming Leung, et al. “Mental Morbidities and Chronic Fatigue in Severe Acute Respiratory Syndrome Survivors: Long-Term Follow-up.” Arch Intern Med 169 (2009):2142-2147.
- Cheng, Sammy Kin-Wing, Jenny Suk-Kwan Tsang, Kwok-Hung Ku and Chee-Wing Wong, et al. “Psychiatric Complications in Patients with Severe Acute Respiratory Syndrome (SARS) During the Acute Treatment Phase: A Series of 10 Cases.” Br J Psychiatry 184 (2004): 359-360.
- Xie, Qin, Fang Fan, Xue-Peng Fan and Xiao-Jiang Wang, et al. “COVID-19 Patients Managed in Psychiatric Inpatient Settings Due to First-Episode Mental Disorders in Wuhan, China: Clinical Characteristics, Treatments, Outcomes, and our Experiences.” Transl Psychiatry 10 (2020):1-11.
- Beurel, Eléonore, Marisa Toups and Charles B Nemeroff. “The Bidirectional Relationship of Depression and Inflammation: Double Trouble.” Neuron 107 (2020): 234-256.
- Alexander, G Caleb, Kenneth B Stoller, Rebecca L Haffajee and Brendan Saloner. “An Epidemic in the Midst of Pandemic: Opioid use Disorder and COVID-19.” Ann Intern Med 173 (2020): 57-58.
- He, Feng, Yu Deng and Weina Li. “Coronavirus Disease 2019 (COVID-19): What We Know?” J Med Virol 92(2020):719-725.
- Corman, V M, J Lienau and M Witzenrath. “Coronaviren Als Ursache Respiratorischer Infektionen.” In Der Internist 60(2019): 1136-45.
- Naqvi, Ahmad Abu Turab, Kisa Fatima, Taj Mohammad and Urooj Fatima, et al. “Insights into SARS-Cov-2 Genome, Structure, Evolution, Pathogenesis and Therapies: Structural Genomics Approach.” BBA -Molecular Basis of Disease (2020):165878.
- Schoeman Dewald and Burtram C Fielding. “Coronavirus Envelope Protein: Current Knowledge.” Virol J 16(2019):1-22.
- Hamming Inge, Wim Timens, M LC Bulthuis and GJ van Navis. “Tissue Distribution of ACE2 Protein, The Functional Receptor For SARS Coronavirus: A First Step in Understanding SARS Pathogenesis.” J Pathol. 203(2004): 631-637.
- Fan, Caibin, Kai Li, Yanhong Ding and Wei Lu Lu. “ACE2 Expression in Kidney and Testis May Cause Kidney and Testis Damage After 2019-Ncov Infection.” MedRxiv (2020).
- Xia, Huijing and Eric Lazartigues. “Angiotensin-Converting Enzyme 2 in The Brain: Properties and Future Directions.” J Neurochem 107(2008): 1482-1494.
- Buzhdygan, Tetyana P, Brandon J DeOre, Abigail Baldwin-Leclair and Trent A Bullock, et al. “The SARS-Cov-2 Spike Protein Alters Barrier Function In 2D Static and 3D Microfluidic InVitro Models of The Human Blood-Brain Barrier.” Neuroniol Dis 146(2020):105131.
- Baig, Abdul Mannan, Areeba Khaleeq, Usman Ali and Hira Syeda. “Evidence of The COVID-19 Virus Targeting The CNS: Tissue Distribution, Host-Virus Interaction, and Proposed Neurotropic Mechanisms.” ACS Chem Neurosci 11(2020): 995-998.
- Walls, Alexandra C, Young-Jun Park, M Alejandra Tortorici and Abigail Wall, et al. “Structure, Function, and Antigenicity of The SARS-Cov-2 Spike Glycoprotein.” Cell 181(2020):281-292.
- Liu, Zhixin, Xiao Xiao, Xiuli Wei and Jian Li, et al. “Composition and Divergence of Coronavirus Spike Proteins and Host ACE2 Receptors Predict Potential Intermediate Hosts of SARS-Cov-2.” J Med Virol 92(2020):595-601.
- Lu, Roujian, Xiang Zhao, Juan Li and Peihua Niu, et al. “Genomic Characterisation and Epidemiology of 2019 Novel Coronavirus: Implications for Virus Origins and Receptor Binding.” Lancet 395(2020):565-574.
- Rocha, Natalia P, Ana Cristina Simoes E Silva, Tiago RR Prestes and Victor Feracin, et al. “RAS in the Central Nervous System: Potential Role in Neuropsychiatric Disorders.” Curr Med Chem. 25(2018):3333-3352.
- Deffner, Felix, Melanie Scharr, Stefanie Klingenstein and Moritz Klingenstein, et al. “Histological Evidence for the Enteric Nervous System and the Choroid Plexus as Alternative Routes of Neuroinvasion by SARS-Cov2.” Front Neuroanat 14(2020):596439
- Wang, Lei, Yin Shen, Man Li and Haoyu Chuang, et al. “Clinical Manifestations and Evidence of Neurological Involvement In 2019 Novel Coronavirus SARS-Cov-2: A Systematic Review and Meta-Analysis.” J Neurol 267(2020): 2777-2789.
- Achar, Aneesha and Chaitali Ghosh. “COVID-19-Associated Neurological Disorders: The Potential Route of CNS Invasion and Blood-Brain Relevance.” Cells 9(2020):2360.
- Butowt, Rafal and Katarzyna Bilinska. “SARS-Cov-2: Olfaction, Brain Infection, and the Urgent Need for Clinical Samples Allowing Earlier Virus Detection.” ACS Chem Neurosci 11(2020):1200-1203.
- Azkur, Ahmet Kursat, Mübeccel Akdis, Dilek Azkur and Milena Sokolowska, et al. “Immune Response to SARS-Cov-2 and Mechanisms of Immunopathological Changes in COVID-19.” Allergy 75(2020):1564-1581.
- Lindqvist, Daniel, Firdaus S Dhabhar, Synthia H Mellon and Rachel Yehuda, et al. “Increased Pro-Inflammatory Milieu in Combat Related PTSD-A New Cohort Replication Study.” Brain Behav Immun 59(2017):260-264.
- Bersani, Francesco Saverio, Owen M Wolkowitz, Daniel Lindqvist and Rachel Yehuda, et al. “Global Arginine Bioavailability, A Marker of Nitric Oxide Synthetic Capacity, is Decreased in PTSD and Correlated with Symptom Severity and Markers of Inflammation.” Brain Behav Immun 52(2016):153-160.
- Northoff, Georg. What Catatonia can Tell us About "Top-Down Modulation": A Neuropsychiatric Hypothesis. Behav Brain Sci25 (2002): 578-604
- Rossi Silvia, Luca Muzio, Valentina De Chiara and Giorgio Grasselli, et al. “Impaired Striatal GABA Transmission in Experimental Autoimmune Encephalomyelitis.” Brain Behav Immun 25 (2011): 947-56.
- Kajani, Raahil, Austin Apramian, Arturo Vega and Nitin Ubhayakar, et al. “Neuroleptic Malignant Syndrome in a COVID-19 Patient.” Case Reports 88 (2020): 28-29.
- Müller, Norbert. “Inflammation in Schizophrenia: Pathogenetic Aspects and Therapeutic Considerations.” 44 (2018): 973-82.
- Beurel, Eléonore, Marisa Toups and Charles B Nemeroff. “The Bidirectional Relationship of Depression and Inflammation: Double Trouble.” Neuron 107 (2020): 234-56
- Benedetti, Francesco, Veronica Aggio, Maria Luisa Pratesi and Giacomo Greco, et al. “Neuroinflammation in Bipolar Depression.” Front Psychiatry 26 (2020) : 71
- Steardo Jr, Luca, Luca Steardo, Alexei Verkhratsky. “Psychiatric Face of COVID-19.” Transl Psychiatry 10 (2020): 261.
- Li, Geng, Yaohua Fan, Yanni Lai and Tiantian Han, et al. “Coronavirus Infections and Immune Responses.” J Med Virol 92 (2020): 424-32.
- Guo, Xi-Zhi J and Paul G Thomas. “New Fronts Emerge in the Influenza Cytokine Storm.” Semin Immunopathol 39 (2017): 541-50.
- Wan, Suxin, Qingjie Yi, Shibing Fan and Jinglong Lv, et al. “Characteristics of lymphocyte Subsets and Cytokines in Peripheral Blood of 123 Hospitalized Patients with 2019 Novel Coronavirus Pneumonia (NCP).” Med Rxiv 118(2020): 6-14.
- Poyiadji,Neo, Gassan Shahin, Daniel Noujaim and Michael Stone, et al. “COVID-19-Associated Acute Hemorrhagic Necrotizing Encephalopathy: Imaging Features.” Radiology 296 (2020): 119-20
- Wang, Dawei, Bo Hu, Chang Hu and Fangfang Zhu, et al. “Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China.” JAMA323 (2020): 1061-9.
- Marco, Cascella, Michael Rajnik, Arturo Cuomo and Scott C Dulebohn, et al. “Features, Evaluation, and Treatment of Coronavirus (COVID-19).” StatPearls [Internet].
- Murthy, Srinivas, Charles D Gomersall and Robert A Fowler. “Care for Critically Ill Patients With COVID-19.” JAMA 323 (2020): 1499-500
- AI, Casas, Eva Geuss Pamela W M Kleikers and Alexander M Herrmann, et al. “NOX4-Dependent Neuronal Autotoxicity and BBB Breakdown Explain the Superior Sensitivity of the Brain to Ischemic Damage.” Proc Natl Acad Sci USA 114 (2017): 12315-20
- Kellawan, J Mikhail, John W Harrell, Alejandro Roldan-Alzate and Oliver Wieben, et al. “Regional Hypoxic Cerebral Vasodilation Facilitated by Diameter Changes Primarily in Anterior Versus Posterior Circulation.” J Cereb Blood Flow Metab 37 (2017): 2025-2034
- Numagami, Yoshihiro, Alan B Zubrow, Om P Mishra and Maria Delivoria‐Papadopoulos. “Lipid Free Radical Generation and Brain Cell Membrane Alteration Following Nitric Oxide Synthase Inhibition During Cerebral Hypoxia in the Newborn Piglet.” J Neurochem 69 (1997):1542-1547.
- Rosenkrantz, Ted S, J Kubin Om P Mishra, Douglass Smith and Maria Delivoria-Papadopoulos. “Brain Cell Membrane Na+, K+-ATPase Activity Following Severe Hypoxic Injury in the Newborn Piglet.” Brain Res 730 (1996): 52-57.
- Boedtkjer, Ebbe. “Acid–Base Regulation And Sensing: Accelerators and Brakes in Metabolic Regulation of Cerebrovascular Tone.” J Cereb Blood Flow Metab 38 (2018):588-602.
- Mallet, Robert T and Myoung-Gwi Ryou. “Erythropoietin: Endogenous Protection of Ischemic Brain.” Vitam Horm 105 (2017):197-232.
- Tang, Ning, Huan Bai, Xing Chen and Jiale Gong, et al. “Anticoagulant Treatment is Associated with Decreased Mortality in Severe Coronavirus Disease 2019 Patients with Coagulopathy.” J Thromb Haemost 18 (2020):1094-1099.
- Kammerer, Tobias, Valentina Faihs, Nikolai Hulde and Manfred Stangl, et al. “Hypoxic- Inflammatory Responses Under Acute Hypoxia: In Vitro Experiments and Prospective Observational Expedition Trial.” Int J Mol Sci 21 (2020):1034.
- Toraldo, D M, F De Nuccio, M De Benedetto and E Scoditti. “Obstructive Sleep Apnoea Syndrome: A New Paradigm by Chronic Nocturnal Intermittent Hypoxia and Sleep Disruption.” Acta Otorhinolaryngol Ital 35 (2015): 69-74.
- Suresh, Sukanya, Praveen Kumar Rajvanshi and Constance T Noguchi. “The Many Facets of Erythropoietin Physiologic and Metabolic Response.” Front physiol 10 (2020): 1534.
- Sinanović, Osman, Mirsad Muftić and Selma Sinanović. “COVID-19 Pandemia: Neuropsychiatric Comorbidity and Consequences.” Psychiatria Danub 32 (2020): 236-244.
- Roy,Devlina, Ghosh Ritwik, Dubey Souvik and Dubey Mahua Jana, et al. “Neurological and Neuropsychiatric Impacts of COVID-19 Pandemic.” Can J Neurol Sci (2020): 1-16.
Citation: He, Yanfei, Ran Yu and Junlin Ren. “The Correlation between Psychiatric Disorders and COVID-19: A Narrative Review” Clin Schizophr Relat Psychoses 15(2020). Doi: 10.3371/CSRP.HYYR.032521.
Copyright: © 2021 He Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.