Research Article - Clinical Schizophrenia & Related Psychoses ( 2021) Volume 0, Issue 0
Forat H Alsultany, Department of Medical Physics, Al-Mustaqbal University, Babil, Iraq, Email: ahmedhasanmed1978@gmail.com
Received: 03-Sep-2021 Accepted Date: Sep 17, 2021 ; Published: 24-Sep-2021
Abstract
In this work, Sleep Disordered Breathing (SDB) in children that may display a continuum from Simple Snoring (SS) down to marked obstructive sleep apnea and the otolaryngological risk factors of sleep-disordered breathing in otherwise healthy children were studied. A prospective study was conducted in the years 2018, 2019 and 2020 on children aged 2-16 years, who were otherwise healthy, received in the ENT department of Almahawil Hospital for evaluation of snoring and breathing difficulties during sleep. We excluded any participants with Down syndrome, craniofacial anomalies, neuromuscular diseases (including cerebral palsy), obesity and laryngomalacia. All children underwent clinical assessment including; physical examination, lateral neck radiograph-x ray to assess the space behind the nose with standardized history collection. We couldn't use any sleep study like polysomnography because of unavailability in our country. We evaluated 326 children (boys: 176, girls: 150) from January 2018 to December 2020. The enrolled children were 120 (boys: 66, girls: 54) in 2018, 65(boys: 35, girls: 30) in 2019 and 141 (boys: 77, girls: 64) in 2020. The age range from 2 years to 16 years and I ordered them into 2-6, 7-10 and 11-16 years' groups. Results showed that 326 (53.9% boys, 46.1% girls) 258 (79.1%) of the total participants had adenotonsillar hypertrophy, 21(6.5%) had adenoid hypertrophy, 31(9.5%) had allergic rhinitis with or without turbinate hypertrophy and 16 (4.9%) had nasal septal deviation. Regarding the age group, 224 (68.7%) were in 2-6 years' group, 68 (20.8%) were in 7-10 years and 34 (10.5%) were in 11-16 years' group.
Keywords
Sleep-disordered • Breathing • Children • Risk factors
Introduction
Pediatric Sleep-Disordered Breathing (SDB) includes; very prevalent group of growing recognized. However, the diagnosis of this spectrum of respiratory disorders remains incomplete [1]. Upper airway obstruction during sleep may result in cessation (apnoea) or reduction (hypopnoea) and noise generation (snoring) as a result of air flow in the mouth and nostrils. Interruption of air-flow at the mouth and nose in children, associated with abnormal movements of chest and abdomen, can be defined as Obstructive Sleep Apnoea (OSA), while hypopnoea as a 50% or greater decrease in oral/ nasal flow capacity [2]. Previous studies focused only on OSA in children [3,4], recent studies considered the concept of obstructive sleep apnoea as the harshest end of the sleep-disordered breathing continuum include; obstructive hypopnea syndrome, upper airway resistance syndrome, snoring, and OSA [5]. The hallmark of pediatric sleep-disordered breathing is snoring the spread rates of OSA in children approximately 1.2% to 5.7%, while the habitual snoring of children has been reported to be about 27%, according to the distribution of population and diagnostic criteria. The highest of spread in children reach at 2 and 8 years as result of hypertrophy of adenoids and tonsils [6].
Cognitive dysfunction and neurological behavior in children are well reported with SDB. Behavioral dysregulation in children is a well-known fact with SDB that show with increased disorders of conduct, aggression, hyperactivity, and impulsivity. In addition, it has been reported poor academic performance, executive dysfunction, inattention, and memory deficits [7]. Obstructive sleep apnoea can cause hypoxia which may induce pulmonary vasoconstriction, subsequently causing systemic hypertension [8], and corpulmonale and pulmonary hypertension [9] for understanding the pathogenesis of SDB in children, should be the basic concepts of airflow [10,11]. Bernoulli reported that a column of air flowing through a narrow tube has a greater pressure and higher velocity and extend on the lateral walls, while in the narrow of the tube, more air pressure being exerted on the side wall and the velocity increases from within the narrowed lumen decreases. This Venturi effect explains acceleration of air-flow as it passes through a narrowing lumen decreases. These rules can be preforming to the pathophysiology of SDB in children where that the muscles pharyngeal dilator keeps air-way patency by bracing shrinkage during awake. During sleep, the pharyngeal dilator muscles maintain airway patency and remain relaxed as a result of reduce muscle tone which leads to growing air-way resistance [10]. In addition, due to present the supraspinal inhibition at sleep, the intercostal muscles are powerless to compensate and contract for any air-way rising resistance with reduced sensitivity in central chemoreceptor to hypercapnia and hypoxia [11].
The option of Polysomnography (PSG) represents diagnostic test and gold standard which confirms the presence of SDB in children and recodes the level of severity [12]. This overnight exam during which has many physiologic parameters are simultaneously measured including: muscle activity, snoring, cardiac activity, blood gases, sleep stages, and eye movements. It should be done in a sleep center facility dedicated to pediatrics under conditions similar to the child’s sleep environment. Unfortunately, this test is not available in our country, so we couldn't use it in our study.
Materials and Methods
A total of 326 patients of both genders, aged 2-16 years, complained of difficult breathing during sleep or snoring were prospectively assessed in the ENT department of Almahawil Hospital, in the northern part of Babylon governorate from January 2014 to December 2016. When first presented to our department, most of the patients came with features of acute upper respiratory tract obstruction due to infection, allergy with or without turbinate hypertrophy, nasal septal deviation or any combination of these causes. Primarily, we used to prescribe proper medical treatment for the patients, local (nasal drops or nasal spray) and systemic (antibiotics, steroids, antihistamine, analgesic) to be reassessed properly 1-3 weeks later. In this study, all patients the evaluation was performed by a otorhinolaryngologistm. In addition, perform the general physical examination and medical history, otorhinolaryngology assessment and lateral neck radiograph to assess postnasal space. Children with Down syndrome, craniofacial anomalies, neuromuscular diseases (including cerebral palsy), obesity, and patients and patients, who underwent any surgical procedure in the upper air-ways, were all excluded. The nasal airways were carefully checked for any obstructing pathology like deviated septum, polyp or allergic rhinitis with or without turbinate hypertrophy. The condition and the size of palatine tonsils were carefully assessed and divided into four degrees according to Brodsky's classification:
First classification: The tonsils are located slightly outside the tonsil fossa, occupying less than 25% of the area between the oropharynx
Second classification: The tonsils are easily visible, occupying 25% to 50% of the oropharynx.
Third classification: The tonsils occupy 50-75% of the oropharynx
Fourth classification: The tonsils occupy above 75% of the oropharynx
Adenoid hypertrophy usually confirmed by lateral neck radiograph. Plain X –ray or CT of paranasal sinuses were used for some patients with allergic rhinitis, turbinate hypertrophy and/or nasal septal deviation.We couldn't use any sleep study PSG because of unavailability in our country. 326 patients were evaluated (boys :176, girls:150) from January 2014 to December 2016. The enrolled children were 120(boys:66, girls:54) in 2014, 65(boys :35, girls:30) in 2015 and 141 (boys :77, girls:64) in 2016. The age range from 2 years to 16 years and we ordered them into 2-6, 7-10 and 11-16 years' groups.
Results
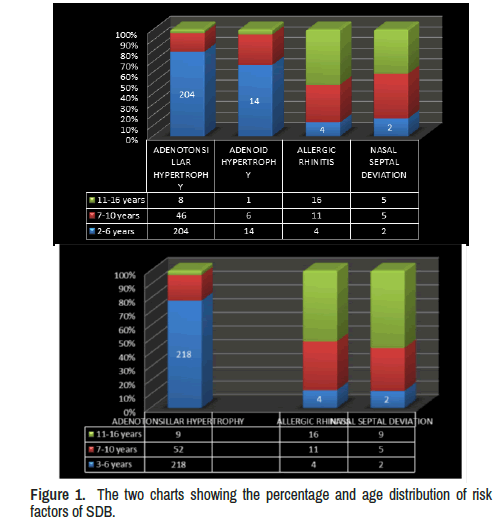
In our study the total participants with SDB were 326 (53.9% boys, 46.1% girls). We've found that 258 (79.1%) had adenotonsillar hypertrophy, from whom 204 were in 2-6 years, 46 in 7-10 years and only 8 in 11-16 years' age groups. 21(6.5%) had adenoid hypertrophy alone, from whom 14 were in 2-6 year, 6 in 7-10 years and only 1 in 11-16 years' age groups. 31(9.5%) had allergic rhinitis with or without turbinate hypertrophy, from whom 4 were in 2-6 years, 11 in 7-10 years and 16 in 11-16 years' age groups. 16(4.9%) had nasal septal deviation, from whom 2 were in 2-6 year, 5 in 7-10 years and 9 in 11-16 years' age groups. Regarding the distribution of the whole patients to the age groups, 224 (68.7) were in 2-6 years' group, 68 (20.8%) were in 7-10years and 34 (10.5%) were in 11-16 years' group. A minority of patients 8 had more than one risk factor (combined), 4 patients with adenotonsillar hypertrophy had also another risk factor, 2 had features of allergic rhinitis and 2 had nasal septal deviation, while 2 patients of allergic rhinitis had also nasal septal deviation and 2 patients of nasal septal deviation had also features of allergic rhinitis. We left them within the group of their main factor.
Discussion
Symptoms of SDB in children can be categorized into:
Night time symptoms: Like snoring, sleeping in unusual positions (with neck extended or fetal posiyion), nocturnal sweating and enuresis (for children above 4 years).
Daytime symptoms: Like inattentiveness, chronic rhinorrhea, learning difficulties, morning headaches, aggressiveness, mouth breathing, anxiety, hyperactivity, deterioration in academic performance, and daytime somnolence (rare in children) [13-19].
Overnight polysomnogram: (PSG; sleep study) is the “gold standard” for classification and diagnosis of SDB in children [20]. As polysomnography is not available in our country, we depend on combination of family observation, clinical ENT evaluation and radiological assessment of the upper airway in screening for clinically significant SDB in children.
Examination: mouth breathing, hyponasal voice and adenoid facies, deviated septum, polyp or allergic rhinitis with or without turbinate hypertrophy. Palatine tonsils moderately to severely enlarged if their size was grade 3 or 4. Adenoidal hypertrophy was assessed by lateral neck radiograph. Plain X –ray or CT of paranasal sinuses may be needed.
Children with adenotonsillar hypertrophy: 258 patients (79.1%) from whom 204(79%) were in 3-6 years, 46 (18%) in 7-10 years and only 8(3%) in 11-16 years' age groups.
Adenoid hypertrophy: Alone is the second group: 21 patients (6.5%), from whom 14(66.6%) were in 3-6 year, 6 (28.6%) in 7-10 years and only 1(4.8%) in 11-16 years' age groups.
We can consider the two groups as adenotonsillar hypertrophy, and in this case the number of patients would be 279 (85.5%). 31 patients (9.5%) had allergic rhinitis with or without turbinate hypertrophy, from whom 4 (13%) were in 3-6 year, 11 (35.5%) in 7-10 years and 16 (51.5%) in 11-16 years' age groups. 16 patients (4.9%) had Nasal septal deviation: From whom 2 (12.5%) were in 3-6 year, 5(31%) in 7-10 years and 9(56.5%) in 11-16 years' age groups. Adenotonsillar hypertrophy forming 279 (85.5%) of the whole patients, the majority of them within the 3-6 years' age group and 7-10 years' age group in the second degree. Adenotonsillar hypertrophy is usually associated with OSA, the severest end of the SDB spectrum, because it involves narrowing of the airway and thus obstruction of the airway during sleep. These children usually presented with mouth breathing, witnessed apnea, abnormal sleep position (hyperextended neck or fetal position), nocturnal enuresis, and daytime somnolence. ENT examination would reveal blocked nose and moderate-severe tonsil enlargement, adenoid hypertrophy confirmed by lateral neck radiograph. Nasal congestion caused by allergies has a significant effect on sleep in both adults and children. Physiologically, nasal breathing is more beneficial during sleep compared with mouth breathing. Mouth breathing, which often results from nasal congestion, is associated with 2.5 times higher total airway resistance [20,21].
In our study 31 patients (9.5%) had clinical features of allergic rhinitis with or without turbinate hypertrophy, from which 4 were in 3-6 year, 11 in 7-10 years and 16 in 11-16 years' age groups. 16 patients (4.9%) had nasal septal deviation, from which 2 were in 3-6 year, 5 in 7-10 years and 9 in 11-16 years' age groups.
The children with nasal obstruction (due to allergic rhinitis with or without turbinate hypertrophy or due to nasal septal deviation) as compared to children with adenotonsillar hypertrophy are milder and with less frequent obstructing features. Witnessed apnea, abnormal sleep position (hyperextended neck or fetal position), nocturnal enuresis, and daytime somnolence were not reported in this group. The quality of research in this area could be improved by using sleep studies primarily to determine the severity of SDB sleep in children [22].
Conclusion
Sleep disordered breathing in children is more common than previously recognized. All children should be screened for snoring as part of routine healthcare and positive findings should be followed by a more detailed evaluation. Adenotonsillar hypertrophy is the leading risk factor of SDB in otherwise normal children. The children with nasal obstruction as compared to children with adenotonsillar hypertrophy are milder and with less frequent obstructing features until a noninvasive, reliable test to diagnose the full spectrum of SDB is available, clinical assessment remains a reliable tool in diagnosing pediatric SDB.
References
- Witmans, Manisha and Rochelle Young. “Update on Pediatric Sleep-Disordered Breathing.” Pediatr Clin North Am 58 (2011): 571-589.
- Loughlin, GM, RT Brouillette, LJ Brooke and JL Carroll, et al. “Standards and Indications for Cardiopulmonary Sleep Studies in Children.” Am J Respir Crit Care Med 153 (1996): 866-878.
- Guilleminault, Christian, Frederic L Eldridge, F Blair Simmons and William C Dement. “Sleep Apnea in Eight Children.” Pediatrics 58 (1976): 23-30.
- Brouillette, Robert T, Sandra K Fernbach and Carl E Hunt. “Obstructive Sleep Apnea in Infants and Children.” J Pediatr 100 (1982): 31-40.
- Messner, Anna H and Rafael Pelayo. “Pediatric Sleep-Related Breathing Disorders.” Am J Otolaryngol 21 (2000): 98-107.
- Montgomery-Downs, Hawley E, Louise M O'Brien and Cheryl R Holbrook, et al. “Snoring and Sleep-Disordered Breathing in Young Children: Subjective and Objective Correlates.” Sleep 27 (2004): 87-94.
- O'Brien, Louise M. “The Neurocognitive Effects of Sleep Disruption in Children and Adolescents.” Sleep Med Clin 6 (2011): 109-116.
- Marcus, Carole L, Mary G Greene and John L Carroll. “Blood Pressure in Children with Obstructive Sleep Apnea.” Am J Respir Crit Care Med 157 (1998): 1098-1103.
- Stradling, JR, G Thomas, ARH Warley and P Williams et al. “Effect of Adenotonsillectomy on Nocturnal Hypoxaemia, Sleep Disturbance, and Symptoms in Snoring Children.” Lancet 335 (1990): 249-253.
- Marcus, Carole L, Eliot S Katz, Janita Lutz and Cheryl A Black, et al. “Upper Airway Dynamic Responses in Children with the Obstructive Sleep Apnea Syndrome.” Pediatr Res 57 (2005): 99-107.
- Isono, Shiroh, Akiko Shimada, Makoto Utsugi and Akiyoshi Konno, et al. “Comparison of Static Mechanical Properties of the Passive Pharynx Between Normal Children and Children with Sleep-Disordered Breathing.” Am J Respir Crit Care Med 157 (1998): 1204-1212.
- American Academy of Pediatrics. “Clinical Practice Guide-Lines: Diagnosis and Management of Childhood Obstructive Sleep Apnea Syndrome.” Pediatrics 109 (2002): 704-712.
- Gozal, David and Dennis W Pope. “Snoring During Early Childhood and Academic Performance at Ages Thirteen to Fourteen Years.” Pediatrics 107 (2001): 1394-1399.
- Ali, NJ, DJ Pitson and JR Stradling. “Snoring, Sleep Disturbance, and Behaviour in 4-5 Year Olds.” Arch Dis Child 68 (1993): 360-366.
- Brooks, Lee J and Howard I Topol. “Enuresis in Children with Sleep Apnea.” J Pediatr 142 (2003): 515-518.
- Kaditis, Athanasios G, Emmanouel I Alexopoulos, Fotini Hatzi and Eleni Kostadima, et al. “Overnight Change in Brain Natriuretic Peptide Levels in Children with Sleep-Disordered Breathing.” Chest 130 (2006): 1377-1384.
- Basha, Suzanne, Christie Bialowas, Kevin Ende and Wasyl Szeremeta. “Effectiveness of Adenotonsillectomy in the Resolution of Nocturnal Enuresis Secondary to Obstructive Sleep Apnea.” Laryngoscope 115 (2005): 1101-1103.
- Gozal, David. “Sleep-Disordered Breathing and School Performance in Children.” Pediatrics 102 (1998): 616-620.
- Castronovo, Vincenza, Marco Zucconi, Luana Nosetti and Carlo Marazzini, et al. “Prevalence of Habitual Snoring and Sleep-Disordered Breathing in Preschool-Aged Children in an Italian Community.”J Pediatr 142 (2003): 377-382.
- American Academy of Sleep Medicine. International Classification of Sleep Disorders. Westchester IL: USA, (2005).
- Craig, Timothy J, Jeffrey L McCann, Faina Gurevich and Michael J Davies. “The Correlation Between Allergic Rhinitis and Sleep Disturbance.” J Allergy Clin Immunol 114 (2004): S139-S145.
- Young, Terry, Larel Finn and Hyon Kim. “Nasal Obstruction as a Risk Factor for Sleep-Disordered Breathing.” J Allergy Clin Immunol 99 (1997): S757-S762.
Citation: H Alsultany Forat and Abdulhusein Mizhir Almaamuri. "Sleep-Disordered Breathing in Children an Overview of Otolaryngological Risk Factors" MClin Schizophr Relat Psychoses 15 S(2021). Doi: 10.3371/CSRP.FAAA.092421
Copyright: © 2021 Alsultany FH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.