Research Article - Clinical Schizophrenia & Related Psychoses ( 2024) Volume 18, Issue 1
Schizophrenia: Origin, History, Prevalence, Symptoms, and Treatment Strategies
Jayarama Reddy*Jayarama Reddy, Department of Biotechnology, St. Joseph’s University, Bengaluru, India, Email: jayaram.reddy@sju.edu.in
Received: 24-May-2024, Manuscript No. CSRP-24-142107; Editor assigned: 27-May-2024, Pre QC No. CSRP-24-142107 (PQ); Reviewed: 11-Jun-2024, QC No. CSRP-24-142107; Revised: 18-Jun-2024, Manuscript No. CSRP-24-142107 (R); Published: 25-Jun-2024, DOI: 10.3371/CSRP.RJ.062524
Abstract
Schizophrenia is a complex psychiatric disorder that has intrigued researchers and clinicians for centuries. This review article delves into the origins and historical evolution of schizophrenia, its prevalence in different populations, the diverse range of symptoms it manifests, and the current treatment approaches available. Understanding these facets is crucial for improving diagnosis, management, and ultimately the quality of life for individuals affected by this challenging condition. Schizophrenia continues to pose significant clinical and societal challenges, necessitating ongoing research and collaborative efforts across disciplines. By advancing our understanding of its origins, prevalence, symptoms, and treatment, we can better support affected individuals and families, ultimately striving towards more effective interventions and improved mental health outcomes. Schizophrenia remains one of the most enigmatic and debilitating mental disorders, affecting approximately 1% of the global population. The lifetime risk of death by suicide in patients with schizophrenia is 5%-10%. Despite therapeutic advancements, challenges such as medication non-adherence, side effects, and stigma associated with schizophrenia persist. Future research aims to refine diagnostic tools, personalize treatment strategies, and explore novel therapeutic targets to improve outcomes and quality of life for individuals living with schizophrenia.
Keywords
Schizophrenia • Mental disorder • Anxiety • Depression • Suicide
Introduction
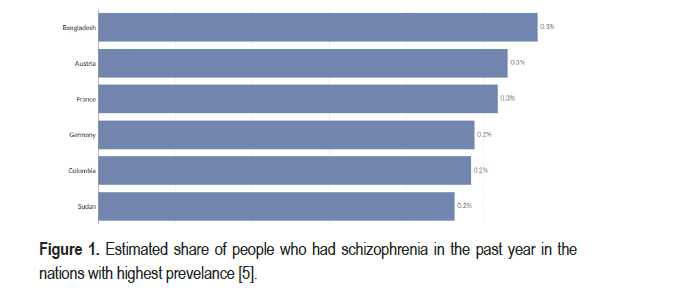
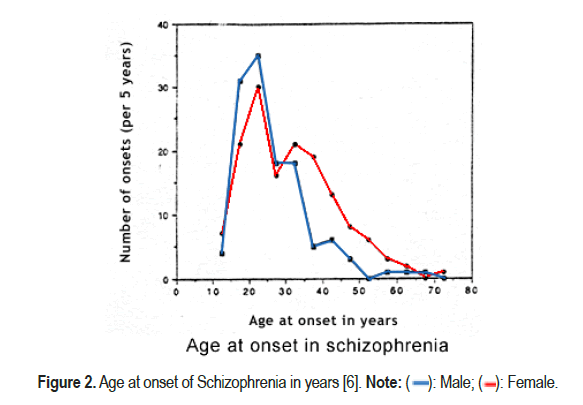
Mental health is being recognised as one of the priority areas in health policies around the world and has also been included in the sustainable development goals [1-3]. Schizophrenia remains one of the most enigmatic and debilitating mental disorders, affecting approximately 1% of the global population [4]. Despite extensive research, its exact etiology remains elusive, contributing to the ongoing challenges in its diagnosis and treatment. At any given time, more than 3 million people in India suffer from schizophrenia. Bangladesh records highest rate of prevalence as shown in Figure 1 [5]. The age of onset of the disorder is higher in males as compared to females as shown in Figure 2 [6]. Originally termed dementia praecox by Emil Kraepelin in the late 19th century, the disorder was later differentiated from other psychoses by Eugen Bleuler in the early 20th century [7]. Historical perspectives have shaped diagnostic criteria and treatment modalities, reflecting evolving societal attitudes towards mental illness. Schizophrenia exhibits a global distribution, although prevalence rates vary across different regions and demographic groups [8,9]. Factors such as genetic predisposition, environmental influences, and socio- economic status play significant roles in its incidence and prevalence.
Figure 1. Estimated share of people who had schizophrenia in the past year in the nations with highest prevelance [5].
Figure 2. Age at onset of Schizophrenia in years [6]. Note: (  ): Male; (
): Male; ( ): Female.
): Female.
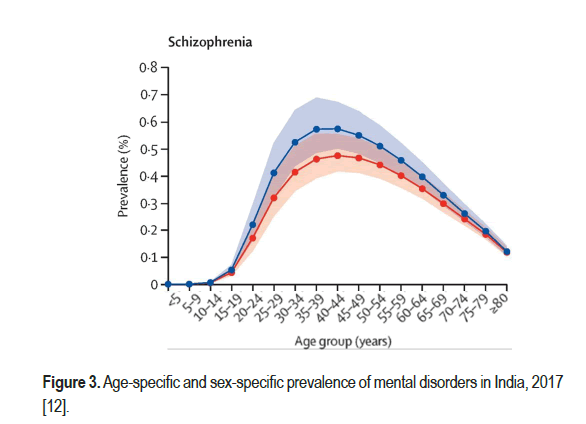
The hallmark symptoms of schizophrenia are categorized into positive symptoms (e.g., hallucinations, delusions), negative symptoms (e.g., social withdrawal, reduced emotional expression), and cognitive deficits (e.g., impaired executive function, attention deficits). Diagnosis is primarily clinical, relying on standardized criteria such as those outlined in the DSM- 5 and ICD-10 [10]. The lifetime risk of death by suicide in patients with schizophrenia is 5% to 10% [11]. Schizophrenia has unfortunately become deeply stigmatized within all societies, especially in countries like India. There are several associated disorders in the patients diagnosed with schizophrenia as shown in Figure 3 [12].
Figure 3.Age-specific and sex-specific prevalence of mental disorders in India, 2017 [12].
Current research implicates abnormalities in neurotransmitter systems (e.g., dopamine, glutamate), neurodevelopmental factors, and structural brain abnormalities in the pathophysiology of schizophrenia. Advances in neuroimaging techniques have provided insights into these underlying biological mechanisms. Management of schizophrenia typically involves a multimodal approach combining antipsychotic medications, psychosocial interventions, and supportive therapies [13]. First-generation (typical) and second-generation (atypical) antipsychotics target dopaminergic pathways, while newer treatments focus on enhancing cognitive function and addressing treatment-resistant symptoms [14].
Literature Review
Prevalence and global statistics
Schizophrenia is a significant global health concern, with varying prevalence rates observed across different regions and populations [15]. Here's an overview of the prevalence and estimated number of cases of schizophrenia both worldwide and specifically in India.
Worldwide prevalence: Globally, schizophrenia affects approximately 20 million people. The prevalence is estimated to be around 0.3% to 0.7% of the population but the rates can vary based on factors such as urbanization, socio-economic status, and access to healthcare. Regions with higher rates include Europe and the Americas, while lower rates are typically seen in Africa and Asia.
Prevalence in India: In India, the prevalence of schizophrenia is reported to be around 0.5% to 1% of the population. With India's large population, this translates to a substantial number of individuals affected by the disorder. Urban areas may have slightly higher prevalence rates compared to rural areas, influenced by factors such as stress, lifestyle changes, and access to mental health services.
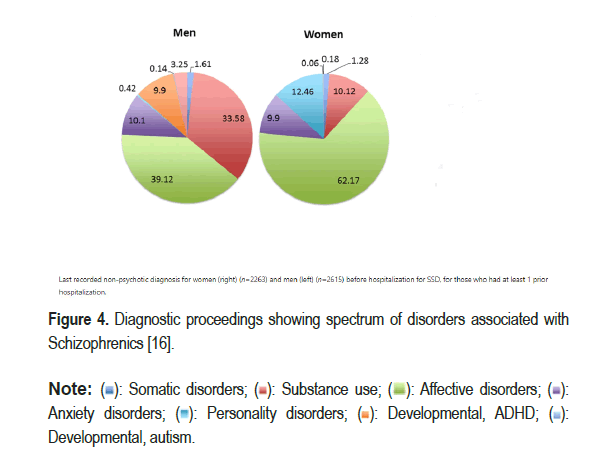
Number of cases: Given the global population of approximately 7.9 billion, and assuming a conservative prevalence rate of 0.5%, there would be around 39.5 million people worldwide affected by schizophrenia. In India, with a population of over 1.3 billion, a prevalence rate of 0.5% would mean around 6.5 million people living with schizophrenia as shown in Figure 4 [16].
Figure 4.Diagnostic proceedings showing spectrum of disorders associated with Schizophrenics [16].
Note: (  ): Somatic disorders; (
): Somatic disorders; ( ): Substance use; (
): Substance use; (  ): Affective disorders; (
): Affective disorders; (  ):Anxiety disorders; (
):Anxiety disorders; ( ): Personality disorders; (
): Personality disorders; (  ): Developmental, ADHD; (
): Developmental, ADHD; (  ): Developmental, autism.
): Developmental, autism.
Factors influencing prevalence
The prevalence of schizophrenia is influenced by various factors, including urbanization, socio-economic conditions, and cultural and genetic predispositions. These elements interplay to shape the susceptibility and presentation of the disorder in different populations.
Urbanization and lifestyle: Urban areas tend to have higher rates of schizophrenia possibly due to higher stress levels, pollution, and lifestyle changes.
Socio-economic factors: Poverty and lack of access to healthcare can impact prevalence rates.
Cultural and genetic factors: Genetic predisposition combined with cultural factors may influence susceptibility and presentation of symptoms.
Challenges and implications
Despite these estimates, there are significant challenges in accurately assessing and addressing the burden of schizophrenia due to underreporting, stigma, and varying healthcare infrastructures globally. Efforts in improving awareness, early detection, and access to treatment are crucial in reducing the personal and societal impact of schizophrenia. Understanding the epidemiology of schizophrenia is essential for healthcare planning, resource allocation, and developing effective strategies to support individuals and families affected by this complex mental disorder across the world, including in India.
Positive, negative and cognitive symptoms
Schizophrenia is a complex psychiatric disorder affecting approximately 1% of the global population. Understanding its symptoms is crucial for accurate diagnosis, effective treatment, and improved quality of life for affected individuals [17-20].
Positive symptoms: Positive symptoms refer to abnormal mental experiences or behaviours that are added to a person's normal repertoire these include:
Hallucinations: Perceptions in the absence of external stimuli, commonly auditory but can also be visual, tactile, olfactory, or gustatory.
Delusions: Fixed false beliefs that are not consistent with the individual's cultural or educational background.
Disorganized thinking: Fragmented thought patterns that impair logical reasoning and coherence in speech.
Negative symptoms: Negative symptoms involve deficits in normal emotional and behavioral processes.
Affective flattening: Reduced intensity and range of emotional expression.
Alogia: Impoverished thinking or speech production.
Avolition: Decreased motivation to initiate and sustain goal-directed activities.
Cognitive symptoms: Cognitive symptoms affect various domains of cognitive function.
Impaired working memory: Difficulty in holding and manipulating information over short periods.
Executive dysfunction: Challenges in planning, problem-solving, and cognitive flexibility.
Attentional deficits: Reduced ability to focus and sustain attention.
Diagnostic criteria and assessment
Diagnosis of schizophrenia involves assessing the presence, duration, and impact of these symptoms using standardized criteria such as those outlined in the DSM-5 (Diagnostic and Statistical manual of Mental disorders, Fifth edition) or ICD-10 (International Classification of Diseases, Tenth revision). Clinical interviews, observations, and rating scales are utilized for comprehensive evaluation.
Neurobiological correlates
Underlying neurobiological mechanisms include dysregulation of neurotransmitter systems (e.g., dopamine, glutamate), structural brain abnormalities, and neurodevelopmental factors. Advances in neuroimaging techniques have provided insights into these neural correlates [21].
Differential diagnosis and comorbidities
Distinguishing schizophrenia from other psychiatric disorders with overlapping symptoms (e.g., bipolar disorder, schizoaffective disorder) is crucial for accurate diagnosis and treatment planning. Comorbidities such as substance use disorders and medical conditions may further complicate management.
Discussion
Treatment strategies
Schizophrenia poses significant challenges due to its chronicity, diverse symptomatology, and impact on cognitive and social functioning. Effective treatment strategies are essential to mitigate symptoms and enhance overall well-being. Treatment strategies for schizophrenia have advanced significantly, yet challenges remain in optimizing outcomes and addressing individual needs. Continued research and innovation are critical to expanding therapeutic options, reducing stigma, and improving the lives of individuals affected by this complex mental disorde r [22,23].
Pharmacological interventions antipsychotic medications
First-generation (typical) and second-generation (atypical) antipsychotics are the cornerstone of pharmacological treatment. They primarily target dopamine receptors and alleviate positive symptoms such as hallucinations and delusions. Examples include haloperidol, risperidone, olanzapine, and clozapine. Newer agents aim to minimize side effects such as metabolic disturbances and extrapyramidal symptoms.
Psychosocial therapies Cognitive Behavioural Therapy (CBT)
CBT helps individuals manage symptoms by identifying and modifying dysfunctional thought patterns and behaviours. It is effective in reducing relapse rates and improving coping strategies. Family Therapy: Involves educating families about schizophrenia, improving communication, and providing support to enhance patient outcomes and family functioning.
Social skills training: Teaches practical skills such as interpersonal communication and problem-solving to improve social interactions and functioning in daily life.
Integrated treatment approaches Assertive Community Treatment (ACT): Multidisciplinary teams provide comprehensive support, including medication management, therapy, and social services, to individuals with severe mental illness in community settings. Supported employment and education: Programs assist individuals in obtaining and maintaining employment or pursuing educational goals, promoting independence and self-sufficiency.
Novel and emerging treatments cognitive remediation: Targets cognitive deficits through structured exercises to improve memory, attention, and problem-solving skills. Transcranial Magnetic Stimulation (TMS): Non-invasive brain stimulation may alleviate symptoms in some individuals resistant to traditional therapies. Digital therapeutics: Mobile apps and online platforms offer self-help tools, psychoeducation, and support for symptom management and adherence to treatment.
Challenges in treatment medication adherence: Many individuals with schizophrenia struggle with adherence to medication regimens due to side effects, lack of insight into their illness, or stigma associated with treatment. Treatment resistance: A subset of patients does not respond adequately to available medications, necessitating alternative strategies and ongoing research into novel treatments. Stigma and social isolation: Barriers to accessing care and achieving recovery include societal stigma and limited support networks.
Future directions in research
Tailoring treatments based on genetic, neurobiological, and clinical factors to enhance efficacy and minimize side effects. Neuroscience advances: Understanding the neural circuits and molecular pathways involved in schizophrenia to develop targeted interventions. Early intervention promoting early detection and intervention to improve longterm outcomes and prevent progression of symptoms and disability. Precision medicine is one of the most advanced methods currently used in the treatment of schizophrenia. It involves tailoring treatment strategies to individual patients based on their unique genetic, biomarker, and clinical characteristics. Here are some key aspects of precision medicine in the context of schizophrenia.
Genetic testing: Identifying specific genetic variations that may influence a person’s response to medications used to treat schizophrenia. For example, variations in genes encoding drug-metabolizing enzymes or receptors targeted by antipsychotic medications [24,25].
Biomarkers: Utilizing biomarkers from blood tests, brain imaging, or other diagnostic tools to predict disease progression, treatment response, or potential side effects of medications. For instance, imaging studies might reveal specific patterns of brain activity or structure that could guide treatment decisions [26].
Personalized treatment plans: Developing individualized treatment plans that consider a patient’s genetic profile, biomarker results, medical history, and preferences. This could involve adjusting medication dosages, choosing between different classes of antipsychotic drugs, or incorporating non-pharmacological interventions such as Cognitive Behavioural Therapy (CBT).
Predictive modelling: Using data analytics and machine learning to analyze large datasets of patient information to predict outcomes and personalize treatment recommendations. This approach aims to improve the accuracy of diagnosis and treatment selection.
Targeted therapies: Exploring new treatment options that target specific molecular pathways implicated in schizophrenia, which may be more effective or have fewer side effects compared to traditional treatments.
Longitudinal monitoring: Implementing continuous monitoring of patients’ symptoms, biomarkers, and treatment responses over time to adjust treatment plans as needed and optimize outcomes.
Ethical considerations
Addressing ethical issues such as privacy concerns related to genetic testing, informed consent for using personal data in research, and ensuring equitable access to precision medicine approaches for all patients. Recovery in schizophrenia is a multidimensional concept, several authors have proposed that it should encompass at least two key domains: Clinical remission and social functioning. Prioritizing functional outcomes in therapeutic interventions for schizophrenia is crucial. The modern methods of treatment hold the key in managing schizophrenia effectively. Therefore, measuring treatment response, remission, and functional recovery from this perspective becomes essential. Achieving improved outcomes in schizophrenia requires an integrated and comprehensive approach that includes pharmacotherapy, psychosocial interventions, and consideration of environmental factors [27].
Conclusion
Providing patient-centered care for individuals with schizophrenia requires an interdisciplinary approach. The healthcare team should include psychiatrists, primary care physicians, advanced practitioners, psychologists, nurses, pharmacists, vocational rehabilitation therapists, occupational therapists, and social workers. These professionals must possess a comprehensive understanding of schizophrenia's clinical aspects, encompassing diagnosis, symptom management, and the complexities of psychopharmacological and psychotherapeutic treatments. This expertise is crucial for interpreting psychiatric assessments, identifying a broad spectrum of symptoms, and navigating the challenges presented by both acute and chronic phases of schizophrenia.
Ethical considerations are paramount in the treatment of schizophrenia, particularly in upholding patient autonomy and ensuring informed consent for treatment plans. Interprofessional collaboration is essential, with each team member contributing specialized knowledge and skills to optimize patient care. Effective communication within the team is critical to fostering an environment where information is openly shared, concerns are promptly addressed, and patient-centered strategies are collaboratively developed. Physicians, advanced practitioners, nurses, pharmacists, and other healthcare professionals must collaborate seamlessly to facilitate the patient's journey from diagnosis through treatment and follow-up care. This coordinated approach helps minimize treatment errors, reduce care delays, and enhance overall patient safety. Ultimately, this comprehensive care approach leads to improved outcomes and emphasizes patient-centered care that supports the recovery of individuals living with schizophrenia.
References
- Chokshi, Maulik B, Patil R, Khanna and Sutapa Bandyopadhyay Neogi, et al. "Health Systems in India." J Perinatol 36 (2016): S9-S12.
- Kyu, Hmwe Hmwe, Degu Abate, Kalkidan Hassen Abate and Solomon M Abay, et al. "Global, Regional, and National Disability-Adjusted Life-Years (Dalys) for 359 Diseases and Injuries and Healthy Life Expectancy (HALE) for 195 Countries and Territories, 1990–2017: A Systematic Analysis for the Global Burden of Disease Study 2017." Lancet 392 (2018): 1859-1922.
- " Mental Health Action Plan 2013-2020." World Heal Org (2013).
- Marder, Stephen R, Tyrone D Cannon. "Schizophrenia." N Engl J Med 381 (2019): 1753-1761.
- “Schizophrenia Prevalence, 2021." Glob Burden Dise (2024).
- Sham PC, C J MacLean and K S Kendler. "A Typological Model of Schizophrenia based on Age at Onset, Sex and Familial Morbidity." Acta Psychiatr Scand 89 (1994): 135-141.
- Kahn, Rene S. "On the Origins of Schizophrenia." Am J Psychiatry 177 (2020): 291-297.
- Owen Michael J, Akira Sawa and Preben B Mortensen. "Schizophrenia." Lancet 388 (2016): 86-97.
- "Schizophrenia." Health topics Nat Inst Ment Heal (2022).
- Biedermann, Falko and W Wolfgang Fleischhacker. "Psychotic Disorders in DSM-5 and ICD-11." CNS Spectr 21 (2016): 349-354.
- McCutcheon, Robert A, Tiago Reis Marques and Oliver D Howes. "Schizophrenia-An Overview." JAMA Psychiatry 77 (2020): 201-210.
- Sagar, Rajesh, Rakhi Dandona, Gopalkrishna Gururaj and R S Dhaliwal, et al. "The Burden of Mental Disorders across the States of India: The Global Burden of Disease Study 1990–2017." Lancet Psychiatry 7 (2020): 148-161.
- Hashimoto, Kenji. "Recent Advances in the Early Intervention in Schizophrenia: Future Direction from Preclinical Findings." Curr Psychiatry Rep 21 (2019): 1-9.
- Paris, Joel. "Differential Diagnosis of Borderline Personality Disorder." Psychiatr Clin North Am 41 (2018): 575-582.
- van de Leemput, J, J L Hess, S . Glatt and M T Tsuang. "Genetics of Schizophrenia: Historical Insights and Prevailing Evidence." Adv Genet 96 (2016): 99-141.
- Sommer, Iris E, Jari Tiihonen, Anouk van Mourik and Antti Tanskanen, et al. "The Clinical Course of Schizophrenia in Women and Men-A Nation-Wide Cohort Study." NPJ Schizophr 6 (2020): 12.
- Marder, Stephen R and Brian Kirkpatrick. "Defining and Measuring Negative Symptoms of Schizophrenia in Clinical Trials." Eur Neuropsychopharmacol 24 (2014): 737-743.
- Adida, Marc, J M Azorin, Raoul Belzeaux and Eric Fakra. "Negative Symptoms: Clinical and Psychometric Aspects." Encephale 41 (2015): 6S15-6S157.
- Davis, Justin, Harris Eyre, Felice N Jacka and Seetal Dodd, et al. "A Review of Vulnerability and Risks for Schizophrenia: Beyond the Two Hit Hypothesis." Neurosci Biobehav Rev 65 (2016): 185-194.
- Batinic, Borjanka. "Cognitive Models of Positive and Negative Symptoms of Schizophrenia and Implications for Treatment." Psychiatr Danub 31 (2019): 181-184.
- Kar, Sujita Kumar and Meha Jain. "Current Understandings about Cognition and the Neurobiological Correlates in Schizophrenia." J Neurosci Rural Pract 7 (2016): 412-418.
- Javitt, Daniel C. "Balancing Therapeutic Safety and Efficacy to Improve Clinical and Economic Outcomes in Schizophrenia: A Clinical Overview." Am J Manag Care 20 (2014): S160- S165.
- Stępnicki, Piotr, Magda Kondej and Agnieszka A Kaczor. "Current Concepts and Treatments of Schizophrenia." Molecules 23 (2018): 2087.
- Karayiorgou, Maria and Joseph A. Gogos. "A Turning Point in Schizophrenia Genetics." Neuron 19 (1997): 967-979.
- Consortium, SPGWAS. "Genome-Wide Association Study Identifies Five New Schizophrenia Loci." Nat Genet 43 (2011): 969-976.
- Nikolac Perkovic, Matea, Gordana Nedic Erjavec, Dubravka Svob Strac and Suzana Uzun, et al. "Theranostic Biomarkers for Schizophrenia." Int J Mol Sci 18 (2017): 733.
- Vita, Antonio and Stefano Barlati. "Recovery from Schizophrenia: Is it Possible?." Curr Opin Psychiatry 31 (2018): 246-255.
Citation: Reddy Jayarama. â??Schizophrenia: Origin, History, Prevalence, Symptoms, and Treatment Strategies.â? Clin Schizophr Relat Psychoses 18 (2024). Doi: 10.3371/CSRP.RJ.062524.
Copyright: �© 2024 Reddy J. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.