Research Article - Clinical Schizophrenia & Related Psychoses ( 2022) Volume 0, Issue 0
Impact of Socioeconomic Status on the Outcome of Physical Therapy in Children with Spastic Cerebral Palsy
Zeinab Ahmed Hussein*, Noura Abou El Fotouh Abed El Fatah, Marwa Mahmoud Mahfouz Mahmoud, Doaa Tammam Atia and Doaa Tammam AtiaDepartment of Physical Therapy for Pediatrics, Central Sherbin Hospital, Daqahlia, Egypt
Department of Basic Science, College of Physical Therapy, Deraya University, Minya, Egypt
Department of Physical Therapy for Pediatrics, College of Physical Therapy, Heliopolis University, Cairo, Egypt, Egypt
Department of Physical Therapy for Pediatrics, National Institute of Neuromotor System, General Organization for Teaching Hospitals and Institutes, Cairo, Egypt
Zeinab Ahmed Hussein, Department of Physical Therapy for Pediatrics, College of Physical Therapy, Cairo University, Cairo, Egypt, Email: zienab.ahmed@pt.cu.edu.eg
Received: 04-Apr-2022, Manuscript No. CSRP-21-61966; Editor assigned: 07-Apr-2022, Pre QC No. CSRP-21-61966 (PQ); Reviewed: 25-Apr-2022, QC No. CSRP-21-61966; Revised: 29-Apr-2022, Manuscript No. CSRP-21-61966 (R); Published: 06-May-2022
Abstract
Background: The development of motor functions in children with cerebral palsy is the outcome of several interacting and relating factors, including types of interventions (medical, physical, or surgical), child characteristics, and socializing agents.
Aim of the study: To evaluate the effect of childhood socioeconomic status on the development of gross motor function after physical therapy intervention in children with spastic cerebral palsy
Methods: A cross-sectional study on eighty children (44 boys, 36 girls) with spastic cerebral palsy aged 3.11 ± 0.88 years old. The Gross Motor Function Classification System (GMFCS) and Socio Economic Scale (SES) were used to evaluate the severity of cerebral palsy and selected children's socioeconomic status, respectively. The Gross Motor Function Measure (GMFM-88) was measured twice times with an interval of six months of physical therapy intervention.
Results: The middle and high socioeconomic classes of children with mild and moderate cerebral palsy showed a significant increase in median values of gross motor function compared with the low class. While there is no significant difference in median values of gross motor function according to socioeconomic classes in children with severe cerebral palsy.
Conclusion: The socioeconomic status may enhance the gross motor functions in children with mild and moderate spastic cerebral palsy after physical therapy interventions
Keywords
Cerebral palsy; Spastic; Socioeconomic status; Physical therapy; Gross motor functions
Introduction
Cerebral Palsy (CP) is a neurodevelopmental disorder in 3.6 per 1,000 live births. It results from a non-progressive lesion in early life before the maturation of the central nervous system [1-3]. Spastic cerebral palsy is classified according to topographic distribution to hemiplegia, diplegia, and quadriplegia [4,5]. Motor impairments are the primary manifestation of spastic CP, including abnormal muscle tone, muscle weakness, lack of mobility, balance, and loss of selective motor control and learning [6,7]. Furthermore, ultimate neurological and psychosocial problems such as cognitive and sensory impairments, epilepsy, and nutritional deficiencies frequently accompany CP children. All CP impairments impact families' well-being and societal health care costs [8,9].
Socio Economic Status (SES) is an overall measure of an individual's work experience and family's economic and social position to others [10]. SES is typically categorized into high, middle, and low according to family's income, education, and occupation [11]. Socioeconomic status promotes and socializes health resources and habits by different factors; it is also considered a determinant of physical activity strengthening or disabling physical activity behavior [12,13]. There is a belief that SES is one of the etiological factors and ways to prevent cerebral palsy [14]. The physical therapy interventions usually focus on maintaining and improving quality of life and function in at minimum essential activities such as gross motor functions and preventing secondary complications for children with CP [15,16]. Also, physiotherapists provide parental support that may develop and restore psychological and social well-being in all activities of daily living [17]. International Classification of Functioning Disability and Health (ICF) and dynamic systems theory of motor control and learning define the development of gross motor function due to the interaction of many subsystems to achieve a functional goal and the child's self-organization [18-20]. Different types of interventions represent the task; the child's characteristics demonstrate individual, while the environmental constraint is represented by socioeconomic status. All of that is the factors that interact to promote the motor functional abilities in children with cerebral palsy [18,21]. So, this study aims to evaluate the effect of childhood socioeconomic status on the development of gross motor functions as the primary physical therapy outcome in children with spastic cerebral palsy.
Materials and Methods
Design
A cross sectional study.
Participants
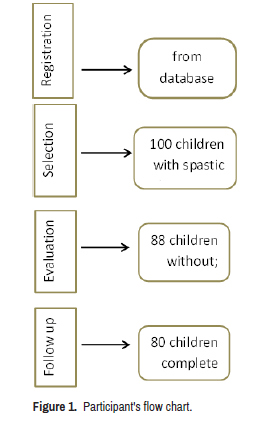
The ethical committee faculty of Physical Therapy Cairo University approved the study (no: P.T.REC/012/001761). Firstly, the files of children were collected from a database of the outpatient clinic faculty of Physical Therapy Cairo University to select children with the following criteria; diagnosed with spastic cerebral palsy, aging from one to four years, while the children who had; preterm birth, genetic disorders, and associated disorders as congenital anomalies, perceptual disorders, or intellectual disorder were excluded. Secondly, the children were eligible for the study; their degree of spasticity, severity level, gross motor functions, and SES was evaluated by a modified Ashworth scale, GMCFS, GMFM, and SES scale. In a follow-up stage after six months of physical therapy interventions, the gross motor functions of the children were reevaluated (Figure 1).
Procedures
Muscle tone assessment: The modified Ashworth scale is a valid and reliable test for measuring the amount of resistance to passive movement [22]. The type of CP was determined as hemiplegia, diplegia, or quadriplegia according to the tone distribution throughout the body.
Severity: Severity is a time-independent variable of age-specific motor activity measured by the Gross Motor Function Classification System (GMFCS). GMFCS is a reliable and valid system to classify the severity of CP. It has five levels of severity (I, II, III, IV and V); levels I and II were grouped as mild category, level III is considered a moderate level, and levels IV and V are severe ones [16].
Gross motor functions: The Gross motor functions were evaluated by Gross Motor Function Measures (GMFM-88). GMFM-88 is a useful clinical assessment tool that consists of 88 items in five dimensions; 1) Lying and Rolling (17 items), 2) Sitting (20 items), 3) Crawling and Kneeling (14 items), 4) Standing (13 items), and 5) Walking, Running and Jumping (24 items) [23]. The total score is the sum of all dimensions divided by five, then calculate the percentage score that ranges from 0 to 100.
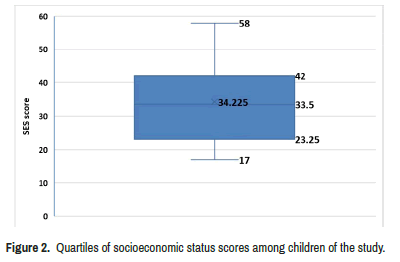
Socio economic status (SES): SES scale was validated and updated on the Socio Economic Status scale for health research [24]. It consists of 7 domains; 1- education and cultural domain (for both husband and wife); 2- family domain; 3- occupation domain; 4- family possessions domain; 5- home sanitation domain; 6- health care domain; 7- economic domain. According to the total scores of socioeconomic statuses, it is classified into four quartiles (very low, low, middle, and high).
Physical therapy program: The physical therapy interventions were based on strength training for all children in the study, improving neuroplasticity through practice and experience [25]. The parents were instructed to stick to sessions as much as possible, three times per week for six months.
Follow up: The scores of GMFM88 were reevaluated after 6 months of a physical therapy program for 80 children to determine the development of gross motor functions.
80 children (44 boys, 36 girls) with spastic cerebral palsy completed the treatment program. Their mean ages were 3.11 ± 0.88 years, classified into three classes (first, second and third). According to tone distribution, the children with diplegia were 52% of all cases, with hemiplegia being 16.3%, while quadriplegia was 31.3% (Figure 2). Quartiles classified the SES of the children into- low, middle, and high (Table 1 and Figure 2).
| GMFM | ||||||||
|---|---|---|---|---|---|---|---|---|
| Age | 1st class (<2.32) (n=20) | 2nd class (2.32 to <3) (n=21) | 3rd class (3≤ 4) (n=39) | X2 | p-value | |||
| ( ± SD) | ||||||||
| 3.11 ± 0.88 | 6.27 | 3.03 | 1.89 | 19.93 | 0.00001* | |||
| Sex | Boys (n=44) | Girls (n=36) | U-value | p-value | ||||
| 2.65 | 2.64 | 791 | ||||||
| Diagnosis | Hemiplegia13 (16.3%) | Diplegia 42 (52.5%) | Quadriplegia25 (31.3%) | X2 | p-value | |||
| 3.44 | 6.05 | 1.13 | 22.42 | 0.0001* | ||||
| SES | Low(<33.5) | Middle (33.5 to 42)+ | High (>42) (n=19) | X2 | p-value | |||
| (n=40) | (n=21) | |||||||
| 2.27 | 6.1 | 4.16 | 8.42 | 0.004* | ||||
Note: Significant : * p value: Probability value, x2: Chi-squared value
Data analysis: The data was collected twice times; before and after six months of the physical therapy program. The descriptive data of all children were treated statistically by means and standard deviations as age and scores of GMFM, quartiles as SES, and frequency as sex, severity, and type of spastic CP. Kruskal-Wallis test was conducted for comparison between several categories. Mann-Whitney U test was conducted for comparison between every two categories. The significance level for all statistical tests was set at P<0.05. The statistics of all measures were performed through the Statistical Package for Social Studies (SPSS) version 22 for windows.
Results
The mean of GMFM percentages before and after 6 months of physical therapy intervention were 47.57 ± 30.26 and 51.51 ± 31.38, respectively with mean difference was -3.94 and the percent of change was 8.28%. That represent a significant increase in GMFM in the study group post treatment (p=0.0001).
Child characteristics and development of motor functions
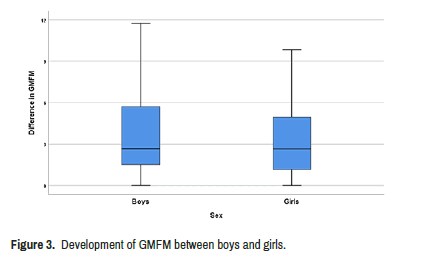
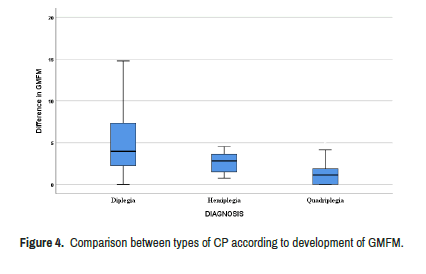
The 1st age class category significantly improved in GMFM scores than other classes. Also, there was no significant difference between boys and girls in the development of motor functions after treatment (p>0.001) (Table 1 and Figure 3). By Mann–Whitney U test, there was insignificant difference of the median of GMFM between diplegia and hemiplegia (p=0.16). When children with diplegia were compared with a quadriplegic, there was a significant increase in the GMFM (p<0.001). Also, there was a significant increase in the mean difference of GMFM in hemiplegia compared with that in quadriplegia (p<0.001) (Table 1 and Figure 4).
Socioeconomic status and development of GMFM
There was a significant difference in the median of GMFM among low, middle, and high SES (p=0.004) . By Mann–Whitney U test, There was a significant increase in median values of GMFM in the middle SES compared with that of high and low SES (p=0.74, p=0.004), and no significant difference between low and high SES (p=0.054). In mild cases of spastic CP, the GMFM significantly improved in middle SES compared to those with high and low SES (p=0.72, p=0.03). In moderate cases: there was a significant difference in median values of GMFM between the groups of SES (p=0.002). There was a significant increase in median values of GMFM in middle and high SES compared with that of low SES (p=0.002) (p=0.01), respectively. in severe cases: There was insignificant difference in median values of GMFM among the groups of SES either low, middle or high (p=0.56) (Table 2).
| GMFM | |||
|---|---|---|---|
| SES | Mild cases (n=26) | Moderate cases (n=29) | Severe cases (n=25) |
| Low | 2.27 | 2.65 | 0.95 |
| (n=13) | (n=15) | (n=12) | |
| Middle | 4.92 | 7.38 | 1.64 |
| (n=5) | (n=8) | (n=8) | |
| High | 3.95 | 8.14 | 1.64 |
| (n=8) | (n=6) | (n=5) | |
| X2 | 4.33 | 12.24 | 1.14 |
| p- value | 0.03* | 0.002* | 0.56 |
| Note: Significant : * p value: Probability value, x2: Chi-squared value | |||
Discussion
The development of motor functions is the primary outcome of physical therapy rehabilitation for children with spastic cerebral palsy, which is considered an increase in GMFM-88 percentages before and after 6 months of physical therapy interventions (the follow-up period). Spasticity is the most severe form of motor impairment in CP, and it represents 72.5% of all CP types [2]. The age was selected to virtuously illustrate the role of parent position in their education, occupation, and income on the outcome of physical therapy intervention. For several reasons;1- below four years old, the primary problems are apparent with few secondary complications, which are considered as a factor of minor influence on the results of physical therapy interventions; 2- the cognitive development in children under four years depend on social learning while older children start to develop self-independent learning experience that explicit the role of SES making less bias in our study; 3- according to emotional development, the children at this age are more autonomy with confidence in the childparent relationship and continued firm parenting helps the child face environmental challenges then learn flexible self-control [25-28]. Generally, after physical therapy intervention, the gross motor functions in all children were significantly improved with a mean difference of 3.94, which might be due to strengthening training which helps improve gross motor function [29].
The current study results showed a significant improvement in GMFM at 1st and 2nd age classes of children with spastic CP after six months of physical therapy intervention than in the 3rd age class. That results point to the early physical therapy intervention may be more effective on the child's outcome, precisely gross motor function, which improves child participation by supporting parents and avoiding the complications. They concluded that marked plastic changes in the brain at an early age have important implications for predicting developmental disorders to encourage functional activities early; otherwise, the child may grow into a functional deficit [30]. The capacity of plasticity in children is more evident in children than in adults, and also it develops structural changes in the brain through motor experiences and parent-child interaction [31]. The percentage of boys in the study group was more than that of girls Figure 3, which is consistent with the previous study mentioned that the incidence of CP is significantly higher in boys than girls due to the biological properties of their brain inducing a greater vulnerability to developing lesions and injuries associated with CP [32]. There is no significant difference between boys and girls in the development of gross motor functions. That results could agree with Mitchell when comparing performances at each level of GMFM or MACS(Manual Ability Classification System) in males and females; there is no significant difference between them. Also, when compared all GMFM and GMFCS among females and males, found that the absence of any statistical gender difference in diplegic and quadriplegic within the total population of children with CP while females in hemiplegic type develop better than boys in standing domain, only [33,34]. The insignificant difference between boys and girls could also be due to young age of participants' because the gender effect becomes more significant as children age and biological diversity become pronounced [35]. There was a significant difference among types of CP ( hemiplegic, diplegic, and quadriplegic) that might be anticipated because all mild cases were hemiplegic in our study. All severe cases were quadriplegic that consistent with the results of Howard who reported that children with level I GMFCS usually have mild spastic hemiplegia and are entirely independent; by contrast, children with level V GMFCS often have severe spastic dyskinesia in a quadriplegic distribution, so they are dependent in mobility [36,37]. The results showed an increase in motor development of children from middle and high socioeconomic classes in a moderate group of CP than those from low one (p=0.002) due to their families' social support. Assis-Madeira suggested that children with moderate CP and low SES were more dependent on their families than children with high SES presenting the necessary skills with help from their caregivers [38]. They found that children from low SES families were neurodevelopmentally delayed twice as those with higher SES [39]. The middle level of SES results showed an insignificant difference with high SES in moderate cases of CP. The results contradict, who concluded a positive association was found between SES and infants' performance on motor scales in other wards as SES increased, the development improved [40,41]. That results were not expected, especially in severe and mild cases, as they contradicted the previous studies on the implications of SES on development found that the families with high SES parents able to invest time and money in their children's development and children from lower SES families at risk for adverse outcomes including poorer health, psychological well-being, and academic achievement. The non-significant difference in motor functions among socioeconomic classes in severe cases of spastic CP may be because all severe cases were quadriplegic cases whose motor development is a little bit improved compared to other types. low social class may neglect those cases because of the needed financial load for continuous management; while those cases in higher classes provide over protection by using facilities and excessive aid, creating greater dependence; however, the social class seems to have no significance in motor development as noticed here [42].
Conclusion
The child′age, sex, severity, diagnosis, and SES are the most common factors which may interfere with the outcome of physical therapy after six months of strengthening training for cerebral palsy. While the level of SES may affect the progress of GMFM in moderated cases of CP aging less than four years. This study was limited by; the small sample size, unequal representation of different types, and different grades of severity of CP only one selection site for patients, and other related factors to SES as nutrition and home bases style were not studied. It was recommended to study the progress of motor functions on other environmental resources and compare the results of nutrition and culture also other child characteristics such as body mass index.
Acknowledgment
We are grateful to all children and parents who participated in this study.
Conflict of Interest
Authors declare that there is no conflict of interest.
REFERENCES
- Mutch, Lesley, Eva Alberman, Bengt Hagberg, and Kazuo Kodama, et al. " Cerebral Palsy Epidemiology: Where Are We Now and Where Are We Going?." Dev Med Child Neurol. 34 (1992): 547-551.
- El-Tallawy, Hamdy N, Wafaa MA Farghaly, Ghaydaa A Shehata, and Tarek A Rageh, et al. " Cerebral Palsy in Al-quseir City, Egypt: Prevalence, Subtypes, and Risk Factors." Neuropsychiatr Dis Treat. 10 (2014): 1267.
- Reeuwijk, Alexander, Petra EM van Schie, Jules G Becher, and Gert Kwakkel. "Effects of Botulinum Toxin Type a on Upper Limb Function in Children with Cerebral Palsy: A Systematic Review." Clin Rehabil 20 (2006): 375-387.
- O'Shea, T Michael, John S Preisser, Kurt L Klinepeter, and Robert G Dillard. " Trends in Mortality and Cerebral Palsy in a Geographically Based Cohort of Very Low Birth Weight Neonates Born Between 1982 to 1994." Pediatrics 10 (1998): 642-647.
- Shams, Aldini ar, and MT Holisaz. "Effect of Sensory Integration Therapy on Gross Motor Function in Children with Cerebral Palsy." 21(2009): 43-48.
- Cvitanović, and P Burić. " Technology-enhanced Upper Limb Physical Rehabilitation in Hemiplegic Cerebral Palsy." Int J Neurorehabilitation 3 (2016): 2376-0281.
- O’Shea, T Michael. " Diagnosis, Treatment, and Prevention of Cerebral Palsy in Near-term/Term Infants." Clin Obstet Gynecol 51 (2008): 816.
- McCullough, Nichola, Jackie Parkes, Claire Kerr, and Brona C McDowell. " The Health of Children and Young People with Cerebral Palsy: A Longitudinal, Population-based Study." Int J Nurs Stud 50 (2013): 747-756.
- Saifi, Saifullah, and Tariq Mehmood. "Effects of Socioeconomic Status on Students Achievement." Int J Soc Sci Res 1 (2011): 119-128.
- Braveman, Paula A, Catherine Cubbin, Susan Egerter, and Sekai Chideya, et al. " Socioeconomic Status in Health Research: One Size Does Not Fit All." Jama 294 (2005): 2879-2888.
- Baker, Elizabeth H. "Socioeconomic Status, Definition." Wiley health 8(2014): 2210-2214.
- Inchley, Joanna C, Dorothy B Currie, Joanna M Todd, and Patricia C et al. "Persistent Socio-demographic Differences in Physical Activity among Scottish Schoolchildren 1990–2002." Eur J Public Health 15 (2005): 386-388.
- Sundrum, R, S Logan, A Wallace, and N Spencer. " Cerebral Palsy and Socioeconomic Status: A Retrospective Cohort Study." Arch Dis Child 90 (2005): 15-18.
- Myklebust, G, R Jahnsen, and S Elkjær. "Registration of Interventions in Children with Cerebral Palsy During Three Years-a Population Based Study." Dev Med Child Neurol 51 (2009): 65.
- Palisano, Robert J, Steven E Hanna, Peter L Rosenbaum, and Dianne J Russell, et al. "Validation of a Model of Gross Motor Function for Children with Cerebral Palsy." Phys Ther 80 (2000): 974-985.
- Anttila, Heidi, Ilona Autti-Rämö, Jutta Suoranta, and Marjukka Mäkelä, et al. "Effectiveness of Physical Therapy Interventions for Children with Cerebral Palsy: A Systematic Review." BMC Pediatr 8 (2008): 1-10.
- WHO. International Classification of Functioning, Disability and Health: ICF. World Health Organization, Geneva, Switzerland (2001).
- Thelen, Esther, and Elizabeth Bates. "Connectionism and Dynamic Systems: Are They Really Different?." Dev Sci 6 (2003): 378-391.
[Crossref], [Google scholar]
- Elman, Jeff. "Development: It's About Time." Dev Sci 6 (2003): 430-433.
- Law, Mary, and Johanna Darrah. "Emerging Therapy Approaches: An Emphasis on Function." J Child Neurol 29(2014): 1101-1107.
- Mutlu, Akmer, Ayse Livanelioglu, and Mintaze Kerem Gunel. "Reliability of Ashworth and Modified Ashworth Scales in Children with Spastic Cerebral Palsy." BMC Musculoskelet Disord 9(2008): 1-8.
[Crossref], [Google scholar]
- El-Gilany, A, A El-Wehady, and M El-Wasify. " Updating and Validation of the Socioeconomic Status Scale for Health Research in Egypt." East Mediterr Health J 18 (2012).
- Palisano, Robert J, Denise M Begnoche, Lisa A Chiarello, and Doreen J Bartlett, et al. " Amount and Focus of Physical Therapy and Occupational Therapy for Young Children with Cerebral Palsy." Phys Occup Ther Pediatr 32 (2012): 368-382.
- Gorter, Jan Willem, Olaf Verschuren, Laura Van Riel, and Marjolijn Ketelaar. " The Relationship Between Spasticity in Young Children (18 Months of Age) with Cerebral Palsy and Their Gross Motor Function Development." BMC Musculoskelet Disord 10 (2009): 1-9.
- Huitt, William, and John Hummel. "Piaget's Theory of Cognitive Development." Edu psychol inter 3 (2003).
[Crossref], [Google scholar]
- Malik, Fatima, and Raman Marwaha. "Developmental Stages of Social Emotional Development in Children." Edu psychol inter 4(2018):113.
- Zoccolillo, Loredana, Daniela Morelli, Febo Cincotti, zand Luca Muzzioli, et al. "Video-game Based Therapy Performed by Children with Cerebral Palsy: A Cross-over Randomized Controlled Trial and a Cross-sectional Quantitative Measure of Physical Activity." Eur J Phys Rehabil Med 51 (2015): 669-676.
- Hadders-Algra, Mijna. "Early Diagnosis and Early Intervention in Cerebral Palsy." Front Neurol 5(2014): 185.
- Kolb, Bryan, Richelle Mychasiuk, Arif Muhammad, and Robbin Gibb. "Brain Plasticity in the Developing Brain." Prog Brain Res 207(2013): 35-64.
- Romeo, Domenico M, Francesca Sini, Claudia Brogna, and Emilio Albamonte, et al. " Sex Differences in Cerebral Palsy on Neuromotor Outcome: A Critical Review." Dev Med Child Neurol 58 (2016): 809-813.
- Mitchell, Louise E, Jenny Ziviani, and Roslyn N Boyd. " Characteristics Associated with Physical Activity among Independently Ambulant Children and Adolescents with Unilateral Cerebral Palsy." Dev Med Child Neurol 57 (2015): 167-174.
- Romeo, Domenico MM, Matteo Cioni, Laura R Battaglia, and Filippo Palermo, et al. "Spectrum of Gross Motor and Cognitive Functions in Children with Cerebral Palsy: Gender Differences." Eur J Paediatr Neurol 15 (2011): 53-58.
- Barnett, Lisa M, Eric Van Beurden, Philip J Morgan,and Lyndon O Brooks, et al. " Gender Differences in Motor Skill Proficiency from Childhood to Adolescence: A Longitudinal Study." Res Q Exerc Sport 81(2010): 162-170.
- Miller, Geoffrey, and Gary D. Clark. The Cerebral Palsies: Causes, Consequences, and Management. Medicine 2(1998): 33.
- Howard, Jason, Brendan Soo, H Kerr Graham, and Roslyn N Boyd, et al. "Cerebral Palsy in Victoria: Motor Types, Topography and Gross Motor Function." J Paediatr Child Health 41 (2005): 479-483.
- Assis-Madeira, Elisângela Andrade, Sueli Galego Carvalho, and Silvana Maria Blascovi-Assis. "Functional Performance of Children With Cerebral Palsy From High and Low Socioeconomic Status." Rev Paul Pediatr 31(2013): 51-57.
- Halpern, Ricardo, ER Giugliani, Cesar G Victora, and Fernando C Barros, et al. "Risk Factors for Suspicion of Developmental Delays at 12 Months of Age." J Pediatr (Rio J) 76 (2000): 421-428.
- Ferreira, Luciana, Ignacio Godinez, Carl Gabbard, and José Luiz Lopes Vieira, et al. " Motor Development in School‐age Children Is Associated with the Home Environment Including Socioeconomic Status." Child Care Health Dev 44 (2018): 801-806.
- Tella, Patricia, Luciane da Rosa Piccolo, Mayra Lemus Rangel, and Luis Augusto Rohde, et al. "Socioeconomic Diversities and Infant Development at 6 to 9 Months in a Poverty Area of São Paulo, Brazil." Psych psycho 40 (2018): 232-240.
- Bradley, Robert H, and Robert F Corwyn. "Socioeconomic Status and Child Development." Annu Rev Clin Psychol 53(2002): 371-399.
- Hackman, Daniel A, and Martha J Farah. "Socioeconomic Status and the Developing Brain." Trends Cogn Sci 13(2009): 65-73.
- Reardon, Sean F. "The Widening Academic Achievement Gap between the Rich and the Poor: New Evidence and Possible Explanations." Whit opp 1(2011): 91-116.
Citation: Hussein, Zeinab Ahmed, Hebatallah Mohamed Kamal, Noura Abou El Fotouh Abed El Fatah, and Marwa Mahmoud Mahfouz Mahmoud, et al. "Impact of Socioeconomic Status on the Outcome of Physical Therapy in Children with Spastic Cerebral Palsy.” Clin Schizophr Relat Psychoses 16S (2022). Doi: 10.3371/CSRP.AZMH.050622
Copyright: © 2022 Hussein ZA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.