Review Article - Clinical Schizophrenia & Related Psychoses ( 2022) Volume 0, Issue 0
Impact of COVID-19 Pandemic on Patients with Schizophrenia Spectrum Disorders: A Review Study
Mina Mohseni1, Payam Khalafi2, Shadi Hajizamani3 and Bahareh Baghchi4*2Department of Psychiatry, Tehran University of Medical Sciences, Tehran, Iran
3Department of Clinical Psychology, Shiraz University, Shiraz, Iran
4Department of Emergency Medicine, Kermanshah University of Medical sciences, Kermanshah, Iran
Bahareh Baghchi, Department of Emergency Medicine, Kermanshah University of Medical sciences, Kermanshah, Iran, Email: bahareh.baghchi@kums.ac.ir
Received: 21-Mar-2022, Manuscript No. CSRP-22-57805; Editor assigned: 23-Mar-2022, Pre QC No. CSRP-22-57805(PQ); Reviewed: 06-Apr-2022, QC No. CSRP-2257805; Revised: 11-Apr-2022, Manuscript No. CSRP-22-57805(R); Published: 18-Apr-2022, DOI: 10.3371/CSRP.MMPK.041822
Abstract
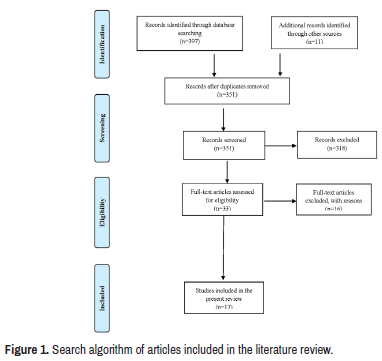
Various measures, including social distancing and quarantine, in order to prevent the progression of the COVID-19 epidemic have led to problems in the community. One of the main consequences of COVID-19 in society is the occurrence of various psychological disorders worldwide. Meanwhile, patients with schizophrenia may be more vulnerable to the effects of COVID-19. Therefore, the present review study was conducted to investigate the effects of the COVID-19 pandemic on patients with schizophrenia spectrum disorders. 408 articles were collected and analyzed from the databases of the MEDLINE, PUBMED, Scopus, Science direct, and EMBASE. A total of 33 papers were evaluated for eligibility, but only 17 articles were included in the study because they met all inclusion criteria. In this review study, it was hypothesized that the restrictions imposed by the prevalence of COVID 19 would lead to adverse effects in patients with schizophrenia. The present study first provides an introduction to COVID-19 disease and the specific conditions created by the epidemic, such as quarantine and social distancing. In the following, we examined the relationship between COVID-19 and the incidence of mental illness. Finally, selected recent studies on the effect of COVID-19 on schizophrenic patients were reviewed in order to conclusion on this subject. A review of the literature on the impact of the COVID-19 epidemic on patients with schizophrenia spectrum disorders showed conflicting results. It was concluded that patients with schizophrenia have a number of risk factors, including social problems and disease-related factors; therefore, these patients may be vulnerable to the effects of the COVID-19 epidemic. On the other hand due to the novelty of the topic, more studies are needed in this field, because these effects seem to be identified in the long term.
Keywords
COVID-19 • Quarantine • Psychological disorders • Schizophrenia
Introduction
On December 31, 2019, Chinese health officials warned the World Health Organization (WHO) about several cases of pneumonia of unknown cause in Wuhan, China. On January 30, 2020, the WHO declared the outbreak a public health emergency of international importance [1]. This acute respiratory illness caused by a new coronavirus (SARS CoV-2), which called COVID-19 by the World Health Organization. Due to its high transmission rate, this disease could affect many people in most parts of the world in a short period of time [2]. China National Health Commission reported 2.1% of deaths among confirmed cases in China as of February 4 [3]. In general, the mortality rate was 11% to 15% among cases admitted to hospitals [4]. Due to the high rate of transmission and mortality rate of COVID-19, extensive studies have been conducted on the prevention of this disease as well as its consequences worldwide.
On the other hand, due to the rapid transmission of the disease, countries around the world have increased their attention to disease monitoring systems [5]. Among the measures taken in this field was legislation on isolation, social and physical distance by imposing restrictions such as home quarantine. The stress associated with the coronavirus epidemic, as well as quarantine condition, have led to increased social stress, which have adverse effects on individuals, especially vulnerable populations, such as patients with schizophrenia spectrum disorders [6]. Studies showed that patients with mental illness have a higher rate of chronic medical illness than the general population. On the other hand, restrictions imposed during the COVID-19 epidemic lead to impaired access to medical care and, consequently, to a worsening of the underlying medical condition in this patient population [7]. Therefore, patients with schizophrenia, especially those with other underlying medical conditions and lifestyle risk factors are at higher risk of developing respiratory infections [8]. Nowadays, there is a great concern about the impact of the COVID-19 epidemic on the mental health of patients with schizophrenia. Due to the fact that some factors related to the COVID-19 pandemic may lead to worsening of mental conditions in patients with schizophrenia, therefore, it is necessary to study the effects of this epidemic on patients with schizophrenia spectrum disorder. A summary of the results of previous studies on the potential impact of COVID-19 pandemic and its implications on patients with schizophrenia spectrum disorders are presented in this review study.
Literature Review
Search strategy
We conducted a comprehensive review of the English language literature involved the impact of COVID-19 on patients with schizophrenia spectrum disorders. The electronic databases MEDLINE, PUBMED, Scopus, Science direct, and EMBASE were searched on August 2021 for reporting the outcomes of the effects of COVID-19 quarantine on patients with schizophrenia. Reference lists of published papers were then also hand-searched in an attempt to identify further reports. The following key words were used: COVID-19; Social isolation; Psychological Disorders; and Schizophrenia. The search terms were then entered onto Google Scholar, to ensure that articles were not missed. Papers were excluded if they were not written in English, lacked documentation, studies without clinical outcomes data, systematic reviews that did not pool data or perform a meta-analysis, and technique articles without outcomes. We then obtained full manuscripts for those studies that met the inclusion criteria. Search algorithm of articles included in the literature review is presented in Figure 1.
COVID-19 global pandemic
In early December 2019, unusual patients with symptoms of pneumonia were observed in Wuhan City, Hubei Province, China, which the causative agent was identified as the Coronavirus (COVID-19). The disease was declared an epidemic on March 11, 2020 by the World Health Organization (WHO) [9]. In studies, the causative agent of Covid-19 disease was identified as a new strain of coronavirus, which was about 79% genetically similar to the causative agent of SARS-COV in 2003 and has a higher pathogenicity, spread rate and transmission [10]. According to statistics provided by the WHO, until July 22, 2020, more than 15 million people have been infected with the virus worldwide and more than 600,000 people have died due to this disease [9]. Therefore, public places were closed in many countries, in order to implement the physical and social distancing to reduce and cut the virus transmission chain [11]. The stress associated with the coronavirus epidemic, as well as measures to limit its prevalence, including quarantine, have led to increased social stress. In this case, some psychologists believe that the occurrence of mental illness will be inevitable in the future population [12].
Psychopathological impact related to COVID-19 physical distancing policies
According to studies conducted during the outbreak of Covid-19, the implementation of physical distance and quarantine has significantly increased anxiety, frustration, uncertainty, depressive symptoms and stress among people [13]. The results of this research show that the mental health of individuals in different countries with different economic, cultural and social status can be affected by COVID-19 epidemic [14]. It is important to identify and assess the extent of mental disorders among people affected by the epidemic in order to provide appropriate solutions to control and reduce them by psychiatrist. The COVID-19 epidemic has had many consequences not only for health, but also for many aspects of life, including the economy, employment, education, and overall quality of life worldwide. The review of the literature showed that decreased sleep quality, increased scores of fear, worry, anxiety and stress, and the occurrence of depressive symptoms from mild to severe among people were significantly affected by the prevalence of COVID-19 [15-21].
Social restrictions and quarantine due to epidemics may have a negative impact on patients with mental disorders. In general, due to the special circumstances of patients with mental disorders, their further limitation may be associated with negative consequences [22]. In addition, social constraints on patients with mental disorders such as schizophrenia may be associated with poor quality of life, economic burden, suicidal ideation, overexposure to stressful situations, and increased risk of drug use, which had negative mental health outcomes can lead to worsening of the condition [23,24]. Therefore, social distancing practices could have a particularly negative impact on individuals with schizophrenia. The results of a study in this field showed that patients with mental illness experience four times more stress in the epidemic than the control group. These people are two to three times more likely to have anxiety and depressive symptoms [25].
Effects of COVID-19 on patients with schizophrenia
Patients with schizophrenia are more likely to develop COVID-19 due to poorer health attention [26]. The increase in these consequences is related to the unfavorable lifestyle and residential instability [27]. Some studies have suggested that patients with schizophrenia have a higher risk of COVID-19 infection due to their increased presence in cumulative conditions [22]. Overall, patients with mental illness, including those with schizophrenia, have a higher rate of chronic medical illness than the general population. Restrictions imposed during the COVID-19 epidemic lead to impaired access to medical care and, consequently, to a worsening of the underlying medical condition in this patients [7]. Patients with schizophrenia, especially those with other underlying medical conditions (cardiovascular disease, diabetes and respiratory diseases) and lifestyle risk factors (high smoking rate, non-compliance with health protocols), are at higher risk of developing respiratory infections [6,8]. Social stressors have adverse effects on individuals, especially vulnerable populations. In the case of the coronavirus pandemic, studies also show that patients with schizophrenia spectrum disorders due to specific disease conditions may be more affected by the epidemic [6].
The results of studies show that patients with schizophrenia are more likely to have negative consequences of the epidemic than other people in the community due to the presence of various risk factors (health and socio-economic risks). In a study in order to investigate the impact of the social distance policies caused by COVID-19 pandemic on patients with schizophrenia, common inflammatory indexes and psychological characteristics were examined [28]. Authors reported that there were no significant differences in changes in schizophrenic symptomatology. However, as mentioned other studies reported different findings, which shows the negative effect of the restrictions imposed by COVID-19 on people with a schizophrenia spectrum disorders [29,30]. Case studies in this field also show an increase in psychosis in this population and even the occurrence of new cases of psychosis in patients without a previous history [31-34]. Therefore, continued psychiatric care and treatment is recommended during the Covid-19 epidemic. A summary of recent studies on the effect of COVID-19 pandemic on patients with schizophrenia spectrum disorders is presented in Table 1. Most studies included review studies, expert opinion, case reports, and treatment guidelines; in other words, no randomized controlled trials were found on this subject [35-39].
|
First Author |
Objective | Conclusion |
|---|---|---|
| Zhand (2021) | Review the impact of the pandemic on patients with schizophrenia |
Patients with schizophrenia spectrum disorders has a number of risk factors, including psychosocial adversities and illness related factors, which may be vulnerable to the effects of the COVID-19 pandemic. |
| Caponnetto (2021) | Investigate what the effects of the pandemic have been on patients with schizophrenia | The research did not confirm the expected results, showing that any kind of worsening of schizophrenic symptomatology Involved the study samples. |
| Rivas-Ramírez (2021) | Rivas-Ramírez (2021) | The prevalence of COVID-19 in hospitalized patients with psychiatric disorders is increased compared with that of the general population; however, a lower mortality rate was detected. Also, an increased risk of COVID-19 was detected in patients with comorbidities. |
| Kozloff (2020) | Investigation of COVID-19 implications for people with Schizophrenia and related disorders | The Covid-19 global epidemic is expected to have a significant effect on patients with schizophrenia and exacerbate their health and economic inequalities. Public health interventions designed to reduce and control the spread of the virus are more likely disproportionately affect people with schizophrenia. |
| Fonseca (2020) | Schizophrenia and COVID-19: Risks and recommendations | The contextual data lead us to infer that there is a greater infection risk in schizophrenia patients. |
| Khosravi (2020) | Introduce the likely challenges for schizophrenic patients during the COVID-19 | Due to the high vulnerability of patients with schizophrenia, it is necessary to consider the needs of these patients during this epidemic. In addition to reducing the burden of the epidemic on schizophrenics, it will also have a positive effect on the whole population. |
| Pinkham (2020) | Comparison of the severity of pre-pandemic symptoms and affective experiences to current symptoms | There were no significant changes in positive, negative, or disorganized symptomatology compared with the pre-pandemic situation in patients with severe mental illnesses. |
| Ma (2020) | Explore the impact of social isolation on common inflammatory indicators and psychological characteristics | Inpatients of schizophrenia suffered from social isolation due to COVID-19 have a severe psychological burden. However, no relevant changes in schizophrenic symptomatology are detected. Social isolation caused patients to develop a weak inflammatory state and led to worse anxiety and sleep quality. |
| Quittkat (2020) | Investigate the perceived impact of Covid-19 and its psychological consequences on people with mental disorders | The symptoms of psychosis, compared to the pre-epidemic situation, do not appear to have changed. Covid-19 may increase the severity of symptoms and psychosocial stress in people with mental disorders. During epidemics, special support is needed to help people with mental disorders and prevent symptoms from getting worse. |
Conclusion
Overall, patients with mental illness, including those with schizophrenia, have a higher rate of chronic medical illness than the general population. Restrictions imposed during the COVID-19 epidemic lead to impaired access to medical care and, consequently, to a worsening of the underlying medical condition in this patient population. The review of the literature on the impact of the COVID-19 epidemic on patients with schizophrenia spectrum disorders showed contradictory results. Some studies did not show a correlation between the psychological effects associated with COVID-19 on schizophrenic patients, but other studies reported different results. In general, due to the fact that patients with schizophrenia have a number of risk factors, including social problems and disease-related factors, these patients may be vulnerable to the effects of the COVID-19 epidemic. On the other hand due to the novelty of the subject, more studies are needed in this field, because these effects seem to be identified in the long term. Therefore, continuous monitoring and long-term studies are required on the impact of the COVID-19 epidemic on this patient population.
Acknowledgements
We would like to thank all those who helped us to conduct this study.
Conflicts of Interest
The authors declare no conflict of interest.
Funding
None.
Ethical Approval
Not required.
References
- Habibzadeh, Parham and Emily K. Stoneman. "The Novel Coronavirus: A Bird's Eye View." Int J Occup Environ Med 11 (2020): 65-71.
[Crossref] [Google scholar] [Pubmed]
- Zhang, Lei and Yunhui Liu. "Potential Interventions for Novel Coronavirus in China: A Systematic Review." J Med Virol 92 (2020): 479-90.
[Crossref] [Google scholar] [Pubmed]
- “National Health Commission (NHC) of the People’s Republic of China.” NHS Press Conference, February (2020).
- Huang, Chaolin, Yeming Wang, Xingwang Li and Lili Ren, et al. "Clinical Features of Patients Infected with 2019 Novel Coronavirus in Wuhan, China." Lancet 395 (2020): 497-506.
[Crossref] [Google scholar] [Pubmed]
- Harapan, Harapan, Naoya Itoh, Amanda Yufika and Wira Winardi, et al. "Coronavirus disease 2019 (COVID-19): A Literature Review." J Infect Public Health 13 (2020): 667-73.
[Crossref] [Google scholar] [Pubmed]
- Kozloff, Nicole, Benoit H. Mulsant, Vicky Stergiopoulos and Aristotle N. Voineskos. "The COVID-19 Global Pandemic: Implications for People with Schizophrenia and Related Disorders." Schizophr Bull 46 (2020): 752-7.
[Crossref] [Google scholar] [Pubmed]
- Melamed, Osnat C., Margaret K. Hahn, Sri Mahavir Agarwal and Valerie H. Taylor, et al. "Physical Health among People with Serious Mental Illness in the Face of COVID-19: Concerns and Mitigation Strategies." Gen Hosp Psychiatry 66 (2020): 30-33.
[Crossref] [Google scholar] [Pubmed]
- Brown, Ellie, Richard Gray, Samantha Lo Monaco and Brian O'Donoghue, et al. "The Potential Impact of COVID-19 on Psychosis: A Rapid Review of Contemporary Epidemic and Pandemic Research." Schizophr Res 222 (2020): 79-87.
[Crossref] [Google scholar] [Pubmed]
- Wang, Cuiyan, Riyu Pan, Xiaoyang Wan and Yilin Tan, et al. "Immediate Psychological Responses and Associated Factors During the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China." Int J Environ Res Public Health 17 (2020): 1729.
[Crossref] [Google scholar] [Pubmed]
- Anand, K. B., S. Karade, S. Sen and R. M. Gupta. "SARS-CoV-2: Camazotz's Curse." Med J Armed Forces India 76 (2020): 136-41.
[Crossref] [Google scholar] [Pubmed]
- Wieczorek, Tomasz, Agata Kolodziejczyk, Marta Ciulkowicz and Julian Maciaszek, et al. "Class of 2020 in Poland: Students’ Mental Health During the COVID-19 Outbreak in an Academic Setting." Int J Environ Res Public Health 18 (2021): 2884.
[Crossref] [Google scholar] [Pubmed]
- Brooks, Megan. “Covid-19: Mental Illness the “Inevitable” Next Pandemic.” Psychiatry News, April, (2020).
- Brooks, Samantha K., Rebecca K. Webster, Louise E. Smith and Lisa Woodland, et al. "The Psychological Impact of Quarantine and How to Reduce it: Rapid Review of the Evidence." Lancet 395 (2020): 912-20.
[Crossref] [Google scholar] [Pubmed]
- Wang, Xiaomei, Sudeep Hegde, Changwon Son and Bruce Keller, et al. "Investigating Mental Health of US College Students During the COVID-19 Pandemic: Cross-sectional Survey Study." J Med Internet Res 22 (2020): e22817.
[Crossref] [Google scholar] [Pubmed]
- Kaparounaki, Chrysi K., Mikaella E. Patsali, Danai-Priskila V. Mousa and Eleni VK Papadopoulou, et al. "University Students’ Mental Health Amidst the COVID-19 Quarantine in Greece." Psychiatry Res 290 (2020): 113111.
[Crossref] [Google scholar] [Pubmed]
- Liu, Shengyi, Ying Liu and Yong Liu. "Somatic Symptoms and Concern Regarding COVID-19 among Chinese College and Primary School Students: A Cross-sectional Survey." Psychiatry Res 289 (2020): 113070.
[Crossref] [Google scholar] [Pubmed]
- Wang, Chongying and Hong Zhao. "The Impact of COVID-19 on Anxiety in Chinese University Students." Front Psychol 11 (2020): 1168.
[Crossref] [Google scholar] [Pubmed]
- Banna, Md Hasan Al, Abu Sayeed, Satyajit Kundu and Enryka Christopher, et al. "The Impact of the COVID-19 Pandemic on the Mental Health of the Adult Population in Bangladesh: A Nationwide Cross-sectional Study." Int J Environ Health Res 32 (2022): 850-61.
[Crossref] [Google scholar] [Pubmed]
- Faisal, Rajib Ahmed, Mary C. Jobe, Oli Ahmed and Tanima Sharker. "Replication Analysis of the COVID-19 Worry Scale." Death Stud 46 (2022): 574-80.
[Crossref] [Google scholar] [Pubmed]
- Ahmed, Oli, Md Zahir Ahmed, Sheikh Md Abu Hena Mostafa Alim and MD Arif Uddin, et al. "COVID-19 Outbreak in Bangladesh and Associated Psychological Problems: An Online Survey." Death Stud 46 (2020): 1080-9.
[Crossref] [Google scholar] [Pubmed]
- Al Zubayer, Abdullah, Md Estiar Rahman, Md Bulbul Islam and Sritha Zith Dey Babu, et al. "Psychological States of Bangladeshi People Four Months after the COVID-19 Pandemic: An Online Survey." Heliyon 6 (2020): e05057.
[Crossref] [Google scholar] [Pubmed]
- Zhand, Naista and Ridha Joober. "Implications of the COVID-19 Pandemic for Patients with Schizophrenia Spectrum Disorders: Narrative Review." BJPsych Open 7 (2021): e35.
[Crossref] [Google scholar] [Pubmed]
- Fonseca, Lais, Elton Diniz, Guilherme Mendonca and Fernando Malinowski, et al. "Schizophrenia and COVID-19: Risks and Recommendations." Braz J Psychiatry 42 (2020): 236-8.
[Crossref] [Google scholar] [Pubmed]
- Hamada, Kareem and Xiaoduo Fan. "The Impact of COVID-19 on Individuals Living with Serious Mental Illness." Schizophr Res 222 (2020): 3-5.
[Crossref] [Google scholar] [Pubmed]
- Iasevoli, Felice, Michele Fornaro, Giordano D'Urso and Diana Galletta, et al. "Psychological Distress in Patients with Serious Mental Illness During the COVID-19 Outbreak and One-month Mass Quarantine in Italy." Psychol Med 51 (2021): 1054-6.
[Crossref] [Google scholar] [Pubmed]
- Shinn, Ann K. and Mark Viron. "Perspectives on the COVID-19 Pandemic and Individuals with Serious Mental Illness." J Clin Psychiatry 81 (2020): 20com13412.
[Crossref] [Google scholar] [Pubmed]
- Druss, Benjamin G. "Addressing the COVID-19 Pandemic in Populations with Serious Mental Illness." JAMA Psychiatry 77 (2020): 891-2.
[Crossref] [Google scholar] [Pubmed]
- Ma, Jun, Tingting Hua, Kuan Zeng and Baoliang Zhong, et al. "Influence of Social Isolation Caused by Coronavirus Disease 2019 (COVID-19) on the Psychological Characteristics of Hospitalized Schizophrenia Patients: A Case-control Study." Transl Psychiatry 10 (2020): 1-5.
[Crossref] [Google scholar] [Pubmed]
- Degnan, Amy, Katherine Berry, Daryl Sweet and Kathryn Abel, et al. "Social Networks and Symptomatic and Functional Outcomes in Schizophrenia: A Systematic Review and Meta-analysis." Soc Psychiatry Psychiatr Epidemiol 53 (2018): 873-88.
[Crossref] [Google scholar] [Pubmed]
- Cranshaw, Thomas and Thiyyancheri Harikumar. "COVID-19 Infection may cause Clozapine Intoxication: Case Report and Discussion." Schizophr Bull 46 (2020): 751.
[Crossref] [Google scholar] [Pubmed]
- Huarcaya-Victoria, Jeff, Dwight Herrera and Claudia Castillo. "Psychosis in a Patient with Anxiety related to COVID-19: A Case Report." Psychiatry Res 289 (2020): 113052.
[Crossref] [Google scholar] [Pubmed]
- Zulkifli, Nathratul Ayeshah, Sulekha Sivapatham and Ng Chong Guan. "Brief Psychotic Disorder in Relation to Coronavirus, COVID-19 Outbreaks: A Case Report." Malaysian J Psychiatry 29 (2020): 67-72. [Crossref]
- Fischer, M., A. N. Coogan, F. Faltraco and J. Thome. "COVID-19 Paranoia in a Patient Suffering from Schizophrenic Psychosis–A Case Report." Psychiatry Res 288 (2020): 113001.
[Crossref] [Google scholar] [Pubmed]
- Ovejero, Santiago, Enrique Baca-García and María Luisa Barrigón. "Coronovirus Infection as a Novel Delusional Topic." Schizophrenia Res 222 (2020): 541-2.
[Crossref] [Google scholar] [Pubmed]
- Caponnetto, Pasquale, Alessandra Benenati and Marilena G. Maglia. "Psychopathological Impact and Resilient Scenarios in Inpatient with Schizophrenia Spectrum Disorders Related to Covid Physical Distancing Policies: A Systematic Review." Behav Sci 11 (2021): 49.
[Crossref] [Google scholar] [Pubmed]
- Rivas-Ramírez, Ángel Roberto, Hiram Tendilla-Beltrán, Laura Eréndira Gómez-Mendoza and Guillermo Loaiza, et al. "Patients with Schizophrenia have Decreased COVID-19 Prevalence among Hospitalised Patients with Psychiatric and Neurological Diseases: A Retrospective Analysis in Mexican Population." Int J Clin Pract 75 (2021): e14528.
- Khosravi, Mohsen. "COVID-19 Pandemic: What are the Risks and Challenges for Schizophrenia." Clin Schizophr Relat Psychoses 27 (2019): 171-8.
- Pinkham, Amy E., Robert A. Ackerman, Colin A. Depp and Philip D. Harvey, et al. "A Longitudinal Investigation of the Effects of the COVID-19 Pandemic on the Mental Health of Individuals with Pre-existing Severe Mental Illnesses." Psychiatry Res 294 (2020): 113493.
[Crossref] [Google scholar] [Pubmed]
- Quittkat, Hannah L., Rainer Düsing, Friederike-Johanna Holtmann and Ulrike Buhlmann, et al. "Perceived Impact of Covid-19 Across Different Mental Disorders: A Study on Disorder-specific Symptoms, Psychosocial Stress and Behavior." Front Psychol 20 (2020): 3256.
[Crossref] [Google scholar] [Pubmed]
Citation: Mohseni, Mina, Payam Khalafi, Shadi Hajizamani and Bahareh Baghchi. “Impact of COVID-19 Pandemic on Patients with Schizophrenia Spectrum Disorders: A Review Study.” Clin Schizophr Relat Psychoses 16S (2022). Doi: 10.3371/CSRP.MMPK.041822.
Copyright: © 2022 Mohseni M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.