Research Article - Clinical Schizophrenia & Related Psychoses ( 2022) Volume 16, Issue 3
Epidemiology of Medical Students Syndrome in Tikrit Medical College
Nahed A. Hassan*Nahed A. Hassan, Department of Medicine, Mcs Community Medicine, Tikrit University College of Medicine, Tikrit, Iraq, Email: drnihadkhalawe@gmail.com
Received: 09-Aug-2022, Manuscript No. CSRP-22-71486; Editor assigned: 12-Aug-2022, Pre QC No. CSRP-22-71486 (PQ); Reviewed: 26-Aug-2022, QC No. CSRP-22-71486; Revised: 01-Sep-2022, Manuscript No. CSRP-22-71486 (R); Published: 09-Sep-2022, DOI: 10.3371/CSRP.HA.090922
Abstract
Background: Medical Student Syndrome (MSS) is a phenomenon whereby medical students experience hypochondriacal symptoms and anxieties relating to the illnesses they are learning about. Anxiety, worry, and depression are all on the rise among medical students around the world. Because of the constant work and numerous examinations, it has been linked to a great deal of psychological stress.
Aim: It is widely acknowledged that medical school can be incredibly stressful and that being under a lot of stress puts one at risk for a variety of psychological and health-related problems. The goal of this study was to see how much worry medical students have about their health.
Materials and Methods: 165 Iraqi undergrad medical students from the University of Tikrit participated in this cross-sectional study, which was conducted utilizing an online self-administrated questionaire using Google form that was disseminated via social media. SPSS version 11.0 was used to examine the data that had been gathered to every analysis.
Results: The study found that the prevalence of MSS among the total sample was 73.9%. Female participants have higher frequency of MSS. The higher prevalence of MSS among students of low socioeconomic states, it was 90%. The Present Study reported that 67,27% of medical students with MSS have a disease- like feeling that keeps them up at night. Prevalence of MSS was higher in clinical Years approximately than in preclinical years.
Conclusion: It can be concluded that because medical students are more susceptible to conditions like Medical Student Syndrome, it is important to inform them of its symptoms and offer them support by addressing various stress-reduction techniques.
Keywords
Medical student's syndrome • Anxiety • Cognitive • Hypochondriasis • Depression • Psychological stress
Introduction
A form of hypochondriasis known as Medical Student Syndrome (MSS) causes health worries mostly related to the illnesses that medical students learn about during their training. Contrary to hypochondriasis, this illness does not lead to an increase in consultations [1].
Many medical students, it is widely believed, develop anxieties and symptoms of illness related to the diseases they are studying at the time, a phenomenon known as "Medical Student Syndrome" [2]. Medical students, particularly those in their second year, have a tendency to diagnose themselves with the illnesses that they are learning about in class. Psychology students develop a similar propensity to attribute personality traits or mood-related habits that they may exhibit to pathology when they are first exposed to the abnormal behavior paper and begin learning about various aspects of psychopathology, and then they diagnose themselves with mental disorders [3]. Medical students are frequently assumed to be predisposed to health worry, referred to as "Medical Student Syndrome" 3.4%, this assumption was founded on the notion that medical research would be preoccupied with diseases that have already been learned. Medical students are also exposed to stress while studying medicine, making them vulnerable to a variety of mental health issues [4].
Students studying medicine are constantly under strain from the fast pace of their education, the hard examinations, the competitive environment, as well as anxiety before and during new clinical experiences [5].
Aim
The goal of this study was to see how much worry medical students have about their health.
Materials and Methods
Case definition
Undergraduate medical students suffering from medical students syndrome.
Study population
165 Iraqi medical undergraduate students participated in the study.
Type of study
Knowledge and the epidemiology of the medical student syndrome were studied cross-sectionally.
Sampling method
Simple random sampling.
Place
Tikrit university college of medicine.
Data collection instrument
The study used a self-administered online Google form questionnaire that was disseminated via social media.
Questionnaire
Data collected by well-designed questionnaire that filled by students through electronic method (facebook, Telegram). The questionnaire was design in English language. It includes close ended questions. It's consists of 16 question related to the study, started with demographic questions by asking about the age, gender and stage of study, socioeconomic status and marital status. The questionnaire also includes did they visit a doctor, how long this feel last, did they use a medication and if the condition cause sleep disturbance.
Ethical consideration
The Medical Research and Ethical Committee of the Faculty of Medicine at Tikrit University gave its approval to this work. Before completing out the questionnaire, verbal agreement was sought from each participant.
Results
The study involved 165 medical students. This study revealed that the overall prevalence of MSS was 73.9% throughout the entire group (122 out of 165 students). However, it was higher among students in the 23 age group to 26 age group (41 out of 49 students, or 83.6%) than among those in the 18 age group to 22 age group (81 out of 116 students, 69.8%). In contrast to male medical students, female participants experience MSS at a higher rate; out of the 98 total female participants, 73(74.4%) are diagnosed with MSS. Regarding marital status, the total number of single medical students 158, while 119(75.3%) of them have MSS. Present study found higher prevalence of MSS among students of low socioeconomic state, it was 90% (Table 1). Out of 122 students with MSS, 69(56.5%) said that they used medication without consulting a doctor. According to the current study, 67.27% of medical students with MSS experience sleep disturbances at night because of their illness. So 40.9% of the students said that the feeling of having a disease lasted for only minutes. Yet 64(52.41%) ignored the symptoms and only 58(47.5%) of respondent investigated their felt Symptoms further (Table 2). The present study identified MSS is higher among nonsmoker students as the prevalence was 96% (Figure 1). The MSS students in the overall sample were divided into preclinical and clinical students according on their stage of study. Approximately 51.6% more people had MSS in clinical years than in preclinical years, which is (48.31%) (Figure 2). The medical condition that caused worries among medical students were cancer (38.8%), heart disease (18.8%), DM (17.6%) and the least worried disease was hypertension (10.9%) (Figure 3).
| Characteristics | Number (%) 165(100%) |
Students with MSS 122(73.9%) | Students without MSS 43(26%) |
|---|---|---|---|
| Age |
116(70.3%) 49(29.6%) |
81(69.8%) 41(83.6%) |
35(30.1%) 8(16.3%) |
| 18-22 23-26 |
|||
| Gender |
67(40.6%) 98(59.3%) |
49(73.1%) 73(74.4%) |
18(26.8%) 25(25.5%) |
| Male Female |
|||
| Marital status |
158(95.7%) 7(4.2%) |
119(75.3%) 3(42.8%) |
39(24.6%) 4(57.1%) |
| Single Married |
|||
| Socioeconomic status High Middle Low |
21(12.7%) 134(81.2%) 10(6%) |
15(71.4%) 98(73.1%) 9(90%) |
6(28.5%) 36(26.8%) 1(10%) |
| Determinant of MSS | Students with MSS N=122 |
|
|---|---|---|
| Have you use medication without consulting a doctor | Yes | 69(56.5%) |
| No | 53(43.4%) | |
| Does the feeling of the disease bother at night sleep | Yes | 82(67.2%) |
| No | 40(32.7%) | |
| How long does the feeling last | Minutes Hours Days Weeks |
50(40.9%) 27(22.1%) 30(24.5%) 15(12.2%) |
| What is your response to stimuli | I ignore | 64(52.4%) |
| Investigate further | 58(47.5%) |
Discussion
The purpose of this study was to detect various psychiatric problems and their associated factors among medical students at Tikrit University. In our study, the fear of being sick is related to the study year. The level of nosophobia exhibited by medical student’s increases with their level of knowledge. This finding's straightforward explanation has to do with the fact that medical students spend more time in their first years studying preclinical sciences and less time studying the clinical illnesses they will study in greater detail in their second and third years of medical school. It seems that higher educational levels of knowledge aid medical students in understanding their symptoms more logically. But as trials move closer to real settings, anxiety levels rise and remain largely stable over the course of the clinical years [5]. According to a study conducted in Pakistan, only a small percentage of medical students with depressive symptoms seek help from doctors or psychologists [6]. According to this study, there is no significant difference between the two groups in terms of disease symptom perception and aid seeking behavior. Similar findings were obtained in a Saudi Arabian study, indicating that help-seeking behavior is unaffected by the type of curriculum pupils are studying [1]. Another study from 2009 found that medical students who are more prone to self-diagnosis tend to modify their diagnoses as they rotate through different hospital departments, implying that self-diagnoses made by students are not a solid criteria for labeling them hypochondriatic [7].
Females were found to have a higher rate of anxiety than males. Female medical students did not have a higher morbidity of psychosomatic issues than male medical students, according to Chinawa, et al. and Puthran, et al. [8,9]. Furthermore, feminization is occurring in medical education as the proportion of female students increases [10,11] and males and females have similar medical objectives [12]. It should be kept in mind that women tend to pay more attention to their own bodies and any illnesses. In contrast to males, they do in fact tend to react to the early stages of sickness more quickly. At the same time, women are characterized by a stronger need to talk about their health with others. Additionally, they choose to speak with a specialist physician more frequently who can address their health concerns. Given that women appear to be more sensitive to alarming signals than men, it is possible that the symptoms of apparent hypochondria in women are also a result of men's widespread misunderstanding of disease symptoms [13].
According to the current study, MSS affects the majority of students from low socioeconomic backgrounds. This was in line with the findings of Eisenberg, et al. who found that kids from low-income homes were significantly more likely to test positive for depression or anxiety disorders, as well as to express suicide thoughts [14]. Unmarried students had a greater rate of MSS prevalence. Sarokhani, et al. found similar results, with single students (39%) having a higher rate of depression than married students (20%) [15]. A medical school as well as other academic departments may experience significant suffering due to the high prevalence of mental health issues among them. Because of this, some authors who have studied this issue contend that everyone who needs support should have access to cheap mental health services at colleges [16].
Practice points
1. Educating others about MSS symptoms and indicators.
2. Counselling sessions for first-year medical students.
3. Support should be provided to students.
4. Different ways for reducing stress should be discussed.
Conclusion
It can be concluded that there is a high prevalence of MSS among medical students. According to the results of the current study, female medical students had a greater degree of MSS than male medical students. The majority of medical students with MSS report night time sleep difficulties as a result of their condition. According to other kids, the impression of having an illness barely lasted a few minutes. The frequency of MSS was higher among clinical year students. Cancer was the most frequent medical condition that caused worry among medical students.
Recommendations
Our data demonstrate that Tikrit health science students have a 73% prevalence of hypochondriac symptoms, indicating that hypochondriasis is a prevalent occurrence that deserves further attention. We propose that universities construct psychological counseling centers for their students. To provide targeted individual assistance, counselors should be able to distinguish hypochondriac symptoms from organic disease and other psychological diseases. An introduction to hypochondriasis should be included in medical education, since this may assist students recognize the problem when it happens during their learning process. To further raise student awareness of the risk of mental health illnesses among them as well as the phenomena of excessive worry related to one's own health, educational programs must also be introduced.
Acknowledgment
First and foremost, we must thank God for all of our blessings. I'd like to thank all of the medical students from the University of Tikrit's College of Medicine who volunteered to participate in this study.
Conflict of Interest
None
Source of Funding
Self-financing
Authors’ Contribution
My efforts went into sample collecting, statistical analysis, and the gathering of scientific materials.
References
- Althagafi, Samiyah Siraj, Maram Hassan AlSufyani, Ola Ahmed Shawky and Omayma Kamel Afifi, et al. "The Health Anxiety in Medical Students, a Comparative Study from Taif University: Medical Student's Syndrome Revisited." Br J Med Pract 12 (2019): a003.
- Waterman, Lauren Z. and John A. Weinman. "Medical Student Syndrome: Fact or Fiction? A Cross-Sectional Study." JRSM Open 5 (2014): 2042533313512480.
[Crossref] [Google scholar] [pubmed]
- Ahmed, Aaiz and S. Samuel. "Self-Diagnosis in Psychology Students." IJIP 5 (2017): 148-64.
- Aulia, Afkar, Carla Raymondalexas Marchira, Irwan Supriyanto and Budi Pratiti. "Cyberchondria in First Year Medical Students of Yogyakarta." J Hum Behav Soc Environ 24 (2020): 1-9.
- Azuri, Joseph, Nissim Ackshota and Shlomo Vinker. "Reassuring the Medical Students’ Disease–Health Related Anxiety among Medical Students." Med Teach 32 (2010): e270-e275.
[Crossref] [Google scholar] [pubmed]
- Zahid, Mohammad Faizan, Ambreen Haque, Moaz Aslam and Numra Abdul Aleem, et al. "Health-Related Anxiety and Hypochondriacal Concerns in Medical Students: A Cross-Sectional Study from Pakistan." Teach Learn Med 28 (2016): 252-9.
[Crossref] [Google scholar] [pubmed]
- Janssens, Thomas, Geert Verleden, Steven De Peuter and Ilse Van Diest, et al. "Inaccurate Perception of Asthma Symptoms: A Cognitive–Affective Framework and Implications for Asthma Treatment." Clin Psychol Rev 29 (2009): 317-27.
[Crossref] [Google scholar] [pubmed]
- Chinawa, J. M., Ada RC Nwokocha, Pius C. Manyike and Awoere Tamunosiki Chinawa, et al. "Psychosomatic Problems among Medical Students: A Myth or Reality?" Int J Ment Health Syst 10 (2016): 1-5.
[Crossref] [Google scholar] [pubmed]
- Puthran, Rohan, Melvyn WB Zhang, Wilson W. Tam and Roger C. Ho. "Prevalence of Depression amongst Medical Students: A Meta‐Analysis." Med Educ 50 (2016): 456-68.
[Crossref] [Google scholar] [pubmed]
- Alers, Margret, Lotte van Leerdam, Patrick Dielissen and Antoine Lagro-Janssen. "Gendered Specialities during Medical Education: A Literature Review." Perspect Med Educ 3 (2014): 163-78.
[Crossref] [Google scholar] [pubmed]
- Pattani, Reena, Christine Marquez, Camellia Dinyarian and Malika Sharma, et al. "The Perceived Organizational Impact of the Gender Gap across a Canadian Department of Medicine and Proposed Strategies to Combat it: A Qualitative Study." BMC Med 16 (2018): 1-10.
[Crossref] [Google scholar] [pubmed]
- Pololi, Linda H., Janet T. Civian, Robert T. Brennan and Andrea L. Dottolo, et al. "Experiencing the Culture of Academic Medicine: Gender Matters, a National Study." J Gen Intern Med 28 (2013): 201-7.
[Crossref] [Google scholar] [pubmed]
- Szczurek, Katarzyna, Natalia Furgał, Dawid Szczepanek and Rashid Zaman, et al. "“Medical Student Syndrome”-A Myth or a Real Disease Entity? Cross-Sectional Study of Medical Students of the Medical University of Silesia in Katowice, Poland." Int J Environ Res Public Health18 (2021): 9884.
[Crossref] [Google scholar] [pubmed]
- Eisenberg, Daniel, Sarah E. Gollust, Ezra Golberstein and Jennifer L. Hefner. "Prevalence and Correlates of Depression, Anxiety, and Suicidality among University Students." Am J Orthopsychiatry 77 (2007): 534-42.
[Crossref] [Google scholar] [pubmed]
- Sarokhani, Diana, Ali Delpisheh, Yousef Veisani and Mohamad Taher Sarokhani, et al. "Prevalence of Depression among University Students: A Systematic Review and Meta-Analysis Study." Depress Res Treat 2013 (2013): 373857.
[Crossref] [Google scholar] [pubmed]
- Gentile, Julie P. and Brenda Roman. "Medical Student Mental Health Services: Psychiatrists Treating Medical Students." Psychiatry 6 (2009): 38.
[Google scholar] [pubmed]
Citation: Hassan, Nahed A. "Epidemiology of Medical Students Syndrome in Tikrit Medical College." Clin Schizophr Relat Psychoses 16 (2022). Doi: 10.3371/CSRP.HA.090922.
Copyright: © 2022 Hassan NA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.







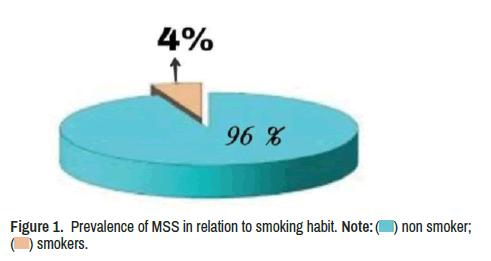
 ) non smoker; (
) non smoker; (  ) smokers.
) smokers.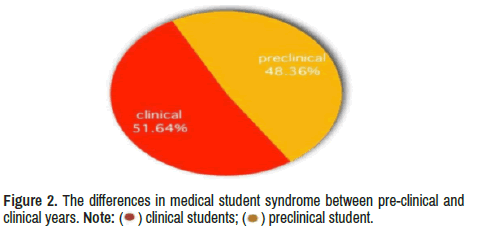
 ) clinical students; (
) clinical students; (  ) preclinical student.
) preclinical student.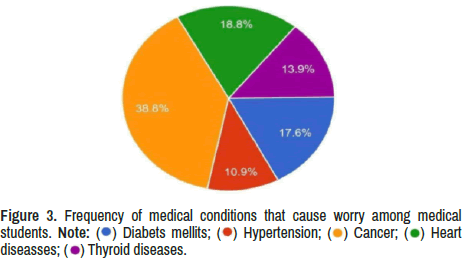
 ) Diabets mellits; (
) Diabets mellits; (  ) Hypertension; (
) Hypertension; (  ) Cancer; (
) Cancer; (  ) Heart
diseasses; (
) Heart
diseasses; (  ) Thyroid diseases.
) Thyroid diseases.