Research - Clinical Schizophrenia & Related Psychoses ( 2021) Volume 0, Issue 0
Comparison Of Dexmedetomidinethiopental And Dexmedetomidineketamine Combinations In Hemodynamic Changes Seizure Durati
Azadeh Abdolvand2Department of Student Research Committee, Arak University of Medical Sciences, Arak, Iran
3Department of Anesthesiology and Critical Care, Arak University of Medical Sciences, Arak, Iran
Alireza Kamali, Department of Anesthesiology and Critical Care, Arak University of Medical Sciences, Arak, Iran, Email: alikamaliir@yahoo.com
Received: 26-May-2021 Accepted Date: Jun 09, 2021 ; Published: 16-Jun-2021, DOI: 10.3371/CSRP.AAJH.140621
Abstract
Introduction: Electroconvulsive therapy is a procedure in which an electrical stimulation of central nervous system is performed to trigger seizure. Seizure duration depends on patient's age, released energy, electrodes location, seizure threshold, prescribed drugs, etc. To prevent different mental-physical damages during ECT, anesthesia and neuromuscular blocking are necessary. Different types of intravenous anaesthetics are used for anesthesia; therefore, the present study aimed to compare dexmedetomidine-thiopental and dexmedetomidine-ketamine combinations in hemodynamic changes, seizure duration, and recovery time in patients candidate for ECT.
Materials and methods: This double-blind clinical trial was conducted on 52 patients, randomly divided into 2 groups. Group 1: Dexmedetomidine-thiopental combination with a dose of 0.5 mg/kg and 1 mg/kg-2 mg/kg of body weight, respectively; Group 2: Dexmedetomidine-ketamine combination with a dose of 0.5 mg/kg and 0.8 mg/kg of body weight, respectively. Recovery time, seizure duration, MAP, PR, blood pressure, and heart rate before and during recovery time were recorded after ECT and seizure. Data were also analyzed by SPSS version 24 software.
Results: No significant difference was observed between the seizure duration in the two groups (27 sec) (P=0.6); however, there was a significant difference between the two groups in terms of recovery time (P=0.001). Recovery time in dexmedetomidine-thiopental group was longer than dexmedetomidine-ketamine group. Although, there was no significant difference between the MAP and PR before ECT in the two groups (P=0.4), MAP and PR in dexmedetomidine-thiopental group (P=0.02) was significantly lower than those of dexmedetomidine-ketamine group (P=0.03). Regarding the patients satisfaction score, there was also no significant difference between the two groups (P=0.4).
Conclusion: The mean PR and MAP were decreased in the dexmedetomidine-thiopental group, however; in the dexmedetomidine-ketamine group, there was a slight increase in the mean PR and MAP. Therefore, dexmedetomidine-ketamine combination could stabilize the hemodynamic without any change in seizure duration and recovery time.
Keywords
Central nervous system • Electrodes • Blood pressure
Introduction
Electro Convulsive Therapy (ECT) is mainly used to treat schizophrenia, major depression, and contraindications such as pregnancy. It is a procedure in which an electrical stimulation of central nervous system is performed to trigger seizure [1]. ECT is used in the treatment of severe mental disorders, particularly major depression, bipolar disorder, and catatonia [2]. The electrical stimulation triggers generalized tonic activity for approximately 10 seconds, followed by diffuse colonic activity, lasting from a few seconds to more than one minute [3]. Anesthetics used in ECT not only reduce physical and psychological trauma but also affect the severity of hemodynamic changes (resulting from parasympathetic and sympathetic discharge) and the seizures duration [4]. Different types anesthetics is used in induction of anesthesia in ECT, including methohexital, sodium thiopental, propofol, etomidate, ketamine, and benzodiazepines. Optimal anesthesia is expected to have minimal hemodynamic changes, fast recovery, few side effects,
and no negative effect on the treatment outcome. Most anesthesiologists prefer sodium thiopental and propofol in ECT, though the effect of these two drugs on the abovementioned parameters is still subject of debate [5]. The ultimate goal of anesthesia in ECT is, therefore, expected to be the rapid induction of anesthesia, muscle relaxation, maintenance of anesthesia depth, maintenance of seizure duration, and fast recovery [6]. With the increased knowledge about the anesthesia aimed to reduce the side effects of ECT, monitoring methods, sedative and musculoskeletal relaxants are considered as the basic components of ECT. Hemodynamic changes after ECT sometimes cause cardiovascular complications and brain events, particularly in the elderly. In this regard, many drugs were studied and the ideal drug was expected to have a rapid effect, does not interfere with the seizure duration, recovery time, and stabilize the hemodynamics [7]. To this end, different complementary drugs such as remifentanil [8] and alpha-2 agonists have been previously used [9].
As a member of alpha-2 agonist family, dexmedetomidine is used in different surgeries to stabilize hemodynamics [10] or, like tizanidine, to control postoperative pain and tremor [11-14]; therefore, the present study aimed to compare dexmedetomidine-thiopental and dexmedetomidineketamine combinations in hemodynamic changes, seizure duration, and recovery time in patients candidate for ECT.
Materials and Methods
This double blind clinical trial was conducted on 52 patients. Based on the inclusion criteria, the target population included all patients candidate for ECT who referred to psychiatric ward of Arak Amir-Kabir Hospital, aged 18- 60 years. A checklist was also used to evaluate the data, and the samples were selected by simple random method using a random number table.
Inclusion criteria
1) Informed consent
2) No history of addiction or medication affecting heart rate and blood pressure
3) ASA-I-II physical status
4) No respiratory and cardiovascular diseases
Exclusion criteria
Patients with a seizure duration of <25 seconds, arrhythmias, and threatening hemodynamic changes during ECT that do not require treatment.
Sample size formula:

Then, 52 patients entered into study and divided into 2 groups. In group 1, after inserting angiocatheter and preparing patient to induction of anesthesia, dexmedetomidine-thiopental combination with a dose of 0.5 mg/kg and 1 mg/kg-2 mg/kg of body weight+succinylcholine chloride and atropine were used. In group 2, dexmedetomidine-ketamine combination with a dose of 0.5 mg/kg and 0.8 mg/kg of body weight+succinylcholine chloride and atropine were used. After induction of complete anesthesia and according to the psychiatrist, 300 joules shock was delivered, then patients entered recovery and oxygen mask were placed on their face. Recovery time, seizure duration, MAP, PR, blood pressure, and heart rate before and during recovery time were recorded after ECT and seizure. Then, the patient satisfaction in postoperative recovery was evaluated (Table 1).
| S. No. | Patient satisfaction in postoperative recovery |
|---|---|
| 1 | Satisfied |
| 2 | No complain |
| 3 | Insufficient satisfaction |
| 4 | Dissatisfaction |
Data analysis
After entering data into SPSS version 24 software, measures of central tendency and dispersion were used to statistically examine the data. Based on the sample size formula, the data were statistically analyzed and then evaluated by independent t-test, paired t-test, and chi-squared test at a significant level of 5%.
Results
Mean age and standard deviation of dexmedetomidine-thiopental and dexmedetomidine-ketamine groups were 2.7 ± 37.8 and 3.2 ± 38.4 years, respectively. In terms of age, there was no statistically significant difference between the two groups (p=0.6).
The number and percentage of gender in dexmedetomidine-thiopental and dexmedetomidine-ketamine groups included 70.7% male and 29.3% female and 71.4% male and 28.6% female, respectively. In terms of gender, there was no statistically significant difference between the two groups (p=0.4).
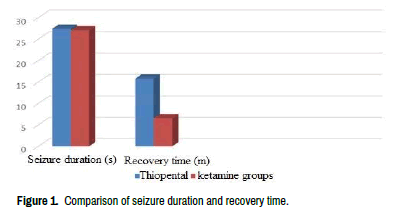
Mean seizure duration and standard deviation of dexmedetomidinethiopental and dexmedetomidine-ketamine groups were 27.4 ± 2.2 seconds and 15.8 ± 1.3 minutes and 27.1 ± 2.8 seconds and 6.57 ± 1.1 minutes, respectively. In terms of seizure duration, there was no statistically significant difference between the two groups (p=0.6). It is while a significant difference was observed between the two groups in terms of recovery time (p=0.001) and dexmedetomidine-thiopental group had a longer recovery time than dexmedetomidine-ketamine group (Figure 1).
Satisfaction score in dexmedetomidine-thiopental and dexmedetomidineketamine groups were 0.98 ± 1.6 and 0.85 ± 1.7, respectively. In terms of satisfaction score, there was no statistically significant difference between the two groups (P=0.4).
As shown in Table 2, there was a significant difference between the MAP in dexmedetomidine-thiopental and dexmedetomidine-ketamine groups (p=0.4) (p=0.03), indicating the increase of MAP after the ECT. However, there was no significant difference between the two groups before and after ECT in terms PR (p=0.1) (p=0.03). Generally, although the seizure duration in the two groups did not change, the recovery time in dexmedetomidinethiopental group was much longer than dexmedetomidine-ketamine group. Also, the two groups had a similar satisfaction score. And in terms of hemodynamics, the mean PR and MAP were decreased in the dexmedetomidine-thiopental group, however; in the dexmedetomidineketamine group, there was a slight increase in the mean PR and MAP.
| Group/Variable | Before ECT | After ECT | p-value |
|---|---|---|---|
| MAP in dexmedetomidine-thiopental | 81.2 ± 4.2 | 80.9 ± 4.1 | P=0.4 |
| PR IN dexmedetomidine-thiopental | 87.3 ± 2.8 | 80.3 ± 3.2 | P=0.07 |
| MAP in dexmedetomidine-ketamine | 79.3 ± 3.4 | 93.9 ± 3.8 | P=0.03 |
| PR in dexmedetomidine-ketamine | 84.2 ± 3.9 | 89.4 ± 4.1 | P=0.1 |
Discussion
Electroconvulsive therapy is a procedure in which an electrical stimulation of central nervous system is performed to trigger seizure. Seizure duration depends on patient's age, released energy, electrodes location, seizure threshold, prescribed drugs, etc. To prevent different mental-physical damages during ECT, anesthesia and neuromuscular blocking are necessary. Different types of intravenous anaesthetics are used for anesthesia; therefore, the present study aimed to compare dexmedetomidine-thiopental and dexmedetomidine-ketamine combinations in hemodynamic changes, seizure duration, and recovery time in patient’s candidate for ECT.
In this study, no significant difference was observed between the seizure duration in the two groups (27 sec) (P=0.6). This was consistent with the results of a study by except that they used only propofol for the induction of anesthesia [15]. In another study by the mean seizure duration in the dexmedetomidine group was longer than the other two groups. Also, the dose of propofol in the dexmedetomidine and midazolam group was lower than other groups. They stated that dexmedetomidine and midazolam
could reduce agitation without side effects [16]. Because of a significant difference between the seizure duration in different groups, their results were not consistent with the results of present study.
In our study, a significant difference was observed between the two groups in terms of recovery time (p=0.001) and dexmedetomidine-thiopental group had a longer recovery time than dexmedetomidine-ketamine group. This was consistent with the results of a study by Fu, et al. except that they used a dose of 1 mg/kg, and their number of samples was small (6 patients receiving 3 to 6 ECT sessions) [17].
Although, there was no significant difference between the MAP and PR before ECT in the two groups (P=0.4), MAP and PR in dexmedetomidinethiopental group (P=0.02) was significantly lower than those of dexmedetomidine-ketamine group (P=0.03). In a study by the administration of dexmedetomidine could prevent high blood pressure in patients treated with ECT [7]. In the study by there was a significant difference between the dexmedetomidine and control groups in terms of MAP at 0,1,3,and 10 minutes, and the MAP in the dexmedetomidine group was lower than the other group [15]. These studies were consistent with our study.
compared the effect of propofol and thiopental on hemodynamic changes and seizure duration in patients candidate for ECT. Our study showed the similar results in hemodynamic changes and seizures duration in ECT using propofol and thiopental. However, time of opening eyes, sitting, and walking without assistance in anesthesia with propofol is shorter than in thiopental. Basically, when ECT is performed in an environment without standard postanesthesia care, propofol is preferable to thiopental because of the faster recovery time [18]. Our study found that dexmedetomidineketamine combination could stabilize hemodynamic without any change in the seizure duration and recovery time.
Conclusion
According to the results, the two groups had a similar satisfaction score. Also, in terms of hemodynamics, the mean PR and MAP were decreased in the dexmedetomidine-thiopental group, however; in the dexmedetomidine-ketamine group, there was a slight increase in the mean PR and MAP. Therefore, dexmedetomidine-ketamine combination could stabilize hemodynamic without any change in the seizure duration and recovery time.
Ethical Considerations
The present study was approved by Ethics Committee of University of Medical Sciences (code of ethics: IR.ARAKMU.REC.1396.176; IRCT code: IRCT201412090202581). In all stages of the study, including writing a proposal, collecting samples, and analyzing the data, the researchers were required to consider ethical principles approved by the Ministry of Health and the Helsinki Declaration. Also, a written consent was obtained from the subjects and they were assured that their information would be treated as strictly confidential.
References
- Jarineshin, Hashem, Saeed Kashani, Fereydoon Fekrat and Majid Vatankhah, et al. “Seizure Duration and Hemodynamic State During Electroconvulsive Therapy: Sodium Thiopental Versus Propofol.” Glob J Health Sci 8 (2016):126.
- Safari, Farhad, Alireza Salimi and Kamran Mottaghi. “Remifentanil in Electro–Convlsive Therapy: A Comparative Double-Blind Study.” J Iran Soci Anaesth Inten Care 2 (2006): 31-35.
- Miller D Ronald. Miller Textbook of Anesthesia. (9th Edtion), Elsevier Churchill Livingstone. USA, (2000).
- Biswas, Saumya, Ratan Kumar Das, Gauri Mukherjee and Tapas Ghose. “Dexmedetomidine an Adjuvant to Levobupivacaine in Supraclavicular Brachial Plexus Block: A Randomized Double Blind Prospective Study.” Ethiop J Health Sci 24 (2014): 203-208.
- Sienaert, Pascal, Manuel Dierick, Gunther Georges Gerard Degraeve and Joseph Peuskens. “Electroconvulsive Therapy in Belgium: A Nationwide Survey on the Practice of Electroconvulsive Therapy.” J Affect Disord 90 (2006): 67-71.
- Boey, Wk and Lai Fan. “Comparison of Propofol and Thiopental as Anaesthetic Agents for Electro Convulsive ?Therapy.” Anaesthesia 45 (2010): 623-628.
- Safari Fatemeh, Salimi Ali and Mottaghi Kamran. “Remifentanil in Electroconvulsive Therapy: A Comparative Double Blind Study.” ?J Iran Soc Anaesthe Intens Care 2 (2016): 5
- Andersen, Jakob , Ulrik Grevstad, Hanna Siegel and Jørgen B Dahl, et al. “Does Dexmedetomidine have a Perineural Mechanism of Action When Used as an Adjuvant to Ropivacaine? A Paired, Blinded, Randomized Trial in Healthy Volunteers.” Anesthesiology 126 (2017): 66-73.
- Butterfield, Noam, Peter Graf, Bernard Macleod and Craig Ries, et al. “Propofol Reduces Cognitive Impairment After Electroconvulsive Therapy.” JECT 20 (2004): 3-9.
- Harti, Abderrazak, B Hmamouchi, Hanane Idali and L Barrou. “Anesthesia for Electroconvulsive Therapy: Propofol Versus Thiopental.” Encephale 27 (2001): 217-22.
- Zaidi, Almas, and Khan F. “Comparison of Thiopental Sodium and Propofol for Electroconvulsive Therapy?.” J Pak Med Assoc 50 (2005): 60-3.
- Villalonga, Andres, Miquel Chajon Gomar and G Fita. “Cardiovascular Response and Anesthetic Recovery in Electroconvulsive Therapy with Propofol or Thiopental.” Convul Ther 9 (2011):17-108.
- Nishihara, Fumio and Shunsuke Saito. “Adjustment of Anaesthesia Depth Using Bispectral Index Prolongs Seizure Duration in Electroconvulsive Therapy.” Anaesthe Intens Care 32 (2004): 661-665.
- Marhofer, David, Stephan Kettner, Peter Marhofer and S Pils, et al. “Dexmedetomidine as an Adjuvant to Ropivacaine Prolongs Peripheral Nerve Block: A Volunteer Study.” Br J Anaesth 110 (2013): 438-442.
- Begec, Zekine, Toprak, Semra Demirbilek and Feray Erdil, et al. “Dexmedetomidine Blunts Acute Hyperdynamic Responses to Electroconvulsive Therapy Without Altering Seizure Duration.” Acta Anaesthesiol Scand 52 (2008): 302-306.
- Mizrak, Ayse, Senem Koruk, Suleyman Ganidagli and Mahmut Bulut, et al. “Premedication with Dexmedetomidine and Midazolam Attenuates Agitation After Electroconvulsive Therapy.” J Anesthesia 23 (2009): 6-10.
- Fu, Wen and Paul White. “Dexmedetomidine Failed to Block the Acute Hyperdynamic Response to Electroconvulsive Therapy.” Anesthesiology 90 (1999): 422-424.
- Haji, Kohan and Naseri Karim. “Propofol and Tiopntal .” Journal of Kordestan University of Medical Sciences 10 (2005):9-15.
Citation: Jamilian,Hamidreza, Anita Alaghemand, Azadeh Abdolvand and Dexmedetomidine-Ketamine Combinations in Hemodynamic Changes, Seizure Duration, and Recovery Time in Patients Candidate for ECT" Clin Schizophr Relat Psychoses 15 S(2021). doi: 10.3371/CSRP.AAJH.140621.
Copyright: © 2021 Jamilian H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.