Research - Clinical Schizophrenia & Related Psychoses ( 2021) Volume 0, Issue 0
Association between Levels of Serum Midkine with Insulin Resistance as New Potential Diagnostic Marker for Thyroid Cancer in its Early Stages
Noor Ali Gebur and Hanaa Addai Ali*Hanaa Addai Ali, Department of Chemistry, College of Science, University of Kufa, Najaf, Iraq, Email: Muthanahana74@gmail.com
Received: 22-Jul-2021 Accepted Date: Aug 05, 2021 ; Published: 12-Aug-2021
Abstract
Background and aim: Thyroid cancer is the most frequent endocrine cancer on the world. This malignancy accounts for 1.3 percent of all cancers and accounts for roughly 0.5 percent of cancer-related deaths worldwide each year. Midkine are implicated in the spread of cancer and orchestrate development, cell survival, neural expansion, and inflammation. Its expression is confined to the kidney, lung, thyroid, and small intestine in healthy adult tissue. In this study, we aimed to evaluate the Serum Midkine in patients with newly diagnosed thyroid cancer, and to identify any correlation with biochemical parameters studied.
Materials and methods: A case-control study design involved 120 Iraqi subjects, 60 of whom had thyroid cancer (48 females and 12 males) to compare the results with 60 healthy adults (50 females and 10 males) whose ages were close to the group of patients ranging from (27-60) years. All subjects' serum levels of Midkine, as well as metabolic indices such as BMI, WHR, (TT3, TT4, TSH), FSG, HOMA-IR, Insulin, QUICKI, C, TG, HDL-C, VLDL-C, LDL-C, and zinc, were measured. The findings were subjected to statistical analysis in order to analyze the differences between the gr5oups tested and to determine the relationship between parameters studied.
Results: According to the statistical analysis, there was no significant difference in mean age between the patients and the control groups. Serum MDK was significantly elevated in thyroid cancer group compared to healthy control groups (202.1 ± 47.4 versus 149.6 ± 41.0 ng/mL, P=0.003), respectively. Serum BMI, TSH, FSG, insulin, HOMA-IR, TC and TG level for thyroid cancer group was significantly higher than healthy control group. However, as compared to the control group, the mean levels of HDL-C, Zinc and QUICKI shown a significant decreased in thyroid cancer group.
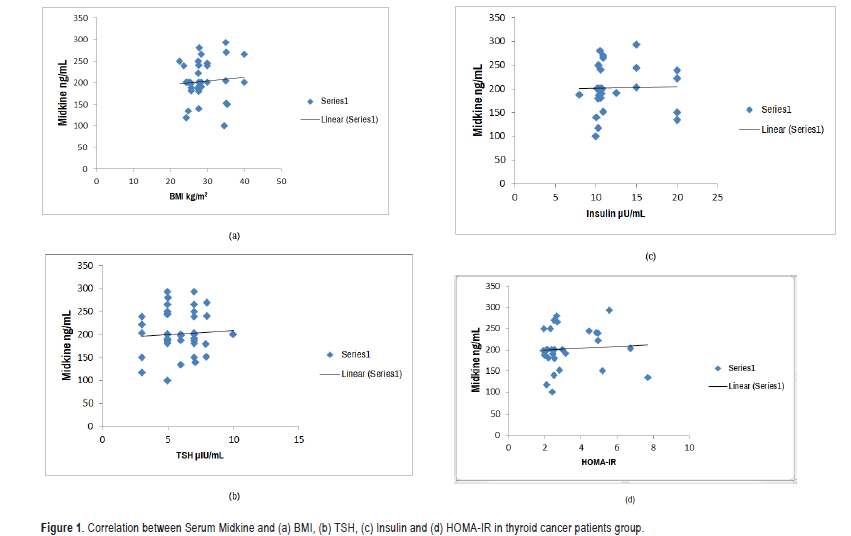
No significant association was found between Midkine and either biochemical parameters studied, except BMI, TSH, insulin and HOMA-IR have a significant positive correlation with Midkine level.
Conclusion: The current investigation found that thyroid cancer patients had considerably higher levels of Midkine than the control group. These results suggest that Midkine may act as a biochemical marker for the early detection and diagnosis of the thyroid cancer.
Keywords
Lipid profile • Midkine • Thyroid cancer • HOMA-IR • QUICKI • Zinc
Introduction
Thyroid cancer is the most frequent endocrine cancer on the planet. This malignancy accounts for 1.3 percent of all cancers and accounts for roughly 0.5 percent of cancer-related deaths worldwide each year. Although differentiated thyroid carcinoma has a low mortality rate, it has a high rate of relapse or persistence, which leads to higher morbidity [1].
Thyroid cancer incidence has increased dramatically worldwide in recent decades [2]. It's unclear if the rise in thyroid cancer is due to greater use of thyroid sonography and sono-guided fine needle aspiration cytology examinations, or if it's due to an actual increase in thyroid cancer caused by an unknown cause. Large tumors have also become more common. Furthermore, despite earlier detection and better treatment, thyroid cancer-related mortality has increased [3]. As a result, variables other than early diagnosis may play a role. Past childhood radiation to the head and neck, family history of thyroid cancer, ionizing radiation exposure [4], and inadequate or excessive iodine consumption are all risk factors for thyroid cancer, which are well-known, but none of them can account for an increase in thyroid cancer cases [5]. Other variables, such as diabetes, obesity, and metabolic syndrome, have been identified [6,7], thyroid cancer has been linked to insulin resistance, chemical toxins and dietary variables [8-12].
Tumor cells, in particular, require a high fatty acid turnover rate to meet the tumor's energetic and synthetic needs [13]. Obesity, as a result, insulin resistance has increased in recent decades, in a similar trend to thyroid cancer [14]. Thyroid hormones affect trace element metabolism, particularly zinc metabolism [15]. In addition, abnormalities in these elements have been linked to goiter and other thyroid diseases, including cancer [16].
The thyroid gland has a higher concentration of trace elements than other tissues, and it has been demonstrated that thyroid hormones influence the metabolism of these elements changes in these components have also been linked to the development of goiter and other thyroid diseases, such as cancer [17]. After removal of the malignant thyroid tissue, Zn serum levels increased dramatically (when compared to pre-operative levels) (p 0.001) [18]. The activity of the enzyme superoxide dismutase (SOD) was dependent on Zn. Changes in this enzyme's activity correspond to changes in Zn serum levels [19].
Midkine (MDK), also known as neurite growth-promoting factor 2 (NEGF2), is a basic heparin-binding growth factor of low molecular weight 13-kDa. MDK was first identified as the Midkine gene product, whose expression increases at early stages of the retinoic acid–induced differentiation of murine to carcinoma stem cells and also in the mid-gestation period of mouse embryogenesis, especially within the kidneys, as a result, the denotation (midgestation, kidney) [20]. It is a highly conserved protein that shares 87 percent of its sequence with mouse Midkine and comprises a family of heparin-binding growth factors with pleiotrophin [21]. Expression of the MDK gene in human adult tissues is extremely low and restricted. Mounting evidence has indicated that MDK plays a significant role in carcinogenesis related activities, such as proliferation, migration, antiapoptosis, mitogenesis, transformation, and angiogenesis, in many types of solid tumors [21,22].
Also it was implicated in the spread of cancer and orchestrates development, cell survival, neural expansion, and inflammation. Its expression is confined to the kidney, lung, thyroid, and small intestine in healthy adult tissue [23]. However, the diagnostic value of serum MDK for thyroid cancer, particularly for those at the early stage, has not yet been investigated in Iraq.
In this study we aimed to evaluate the Serum Midkine in patients with newly diagnosed thyroid cancer.
Materials and Methods
Subjects and study design
All studies were conducted with approvals from the regional ethical committee of University of Kufa, Faculty of Science. Informed consent forms were obtained from each participant before beginning the research. This study was designed as a case control study as two different groups included 120 subjects, 60 thyroid cancer patients (48 females and 12 males), ranging in age from 20 to 60 years. Patients were registered in “Diwaniya Teaching Hospital” in Al-Qadisiyah, Iraq, throughout the period from January 2020 to September 2021. To compare the results, 60 healthy adults were included as a control group. Their ages ranged from 20 to 60 years, similar to the patients' (50 females and 10 males).
Exclusion criteria
Subjects suffered from chronic diseases like diabetes mellitus, cardiovascular diseases, systemic sickness, chronic kidney disease, and smokers were excluded in this study.
Collection of samples
Five milliliters of venous blood were taken from cancer thyroid patients and a healthy group between 8:30 AM and 10:00 AM using antecubital venipuncture using G 23 needles after an 8-12 hour fast. At room temperature, 5 ml of blood was allowed to coagulate in a test tube. After centrifugation at (3000 × g) for 15 minutes, the serum was divided into four tubes and kept at -20°C until analysis.
Anthropometric evaluation
The Body Mass Index was assessment by dividing weight in kilograms by length of individual in square meter: BMI=(weight in kg)/ (height in meters).
Biochemical evaluation
Serum Thyroid-Stimulating Hormone (TSH), Total Triiodothyronine (TT3), and Total Thyroxine (TT4) levels were measured by using ELISA micro plate washer and reader, which is a compact immunoassay system based on the Enzyme Linked Immunosorbent Assay (ELISA) principles, and a commercial kit from CORTEZ (USA). The concentrations of fasting serum glucose, total cholesterol, High Density Lipoprotein Cholesterol (HDL-C), and triglyceride were measured by colorimetric method for quantitative in vitro diagnostic measurement using a commercial kit from LiNEAR (SPAIN). Low Density Lipoprotein Cholesterol (LDL-C) levels were calculated by Fried Ewald’s formula [24]. Serum zinc concentration was measured by using Spectrophotometer advice at (578 nm) using a commercial kit from LTA (Italia). Fasting insulin levels were measured by immunoenzymometric assay (TYPE 3) with a commercial kit from Monobind Inc. (USA). Enzyme-linked immunosorbent assay kits (MELSIN, China) measured Serum Midkine, Insulin resistance was calculated by using homeostasis model assessment (HOMA-IR) score that employs the formula: fasting insulin concentration (μIU/L) glucose (mmoL/L)/22.5. Individuals with HOMA-IR>2.7 were accepted as insulin resistant. QUICKI values (quantitative insulin sensitivity check index) was estimated by equation: QUICKI=1/ log(I0)+log(G0), where I0 is the fasting insulin (μIU/ml), and G0 is the fasting glucose (mg/dL) [25,26].
Bio-statistical analysis
Microsoft Excel 2010 and SPSS-24 (Statistical Package For Social Science-Version 24) software were used to conduct the statistical analysis. The data were subjected to statistical analysis, with the t-test being used to examine the differences between the analyzed groups. Pearson's correlation coefficient was employed to assess the correlation between parameters.
Results
Table 1 show the mean of age has no significant difference between patients group compared with control group. Nevertheless, found the mean of BMI, TSH, FSG, and insulin, HOMA-IR, TC, TG and Midkine levels a significant increase in thyroid cancer group when compared with control group. While, means of serum Zinc, QUICKI, and HDL-C levels in patients group have a significant decrease compared with control group.
| Parameters | Groups | P Value | |
|---|---|---|---|
| Control | Thyroid cancer | ||
| Mean ± SD | Mean ± SD | ||
| (n=30) | (n=60) | ||
| Age (year) | 42.03 ± 7.17 | 43.0 ± 7.20 | 0.148 |
| SBP (Hmmg) | 120.12 ± 9.05 | 130.13 ± 12.05 | 0.01 |
| DBP (Hmmg) | 76.01 ± 0.38 | 78.70 ± 2.38 | 0.054 |
| BMI (Kg/m2) | 24.3 ± 2.0 | 28.2 ± 3.8 | 0 |
| W/H | 0.82 ± 0.19 | 0.88 ± 0.22 | 0.054 |
| TT3 (ng/mL) | 1.92 ± 0.33 | 2.14 ± 0.93 | 0.53 |
| TT4 (ng/mL) | 73.3 ± 12.5 | 88.0 ± 36.2 | 0.108 |
| TSH (µIU/mL) | 2.30 ± 0.81 | 5.56 ± 1.73 | 0.022 |
| FSG (mg/dL) | 82.5 ± 6.38 | 104.3 ± 28.2 | 0.05 |
| Insulin (µU/mL) | 3.92 ± 1.34 | 12.1 ± 3.46 | 0 |
| HOMA-IR | 0.80 ± 0.28 | 3.22 ± 1.54 | 0 |
| QUICKI | 0.47 ± 0.04 | 0.30 ± 0.01 | 0 |
| T-CHO (mg/dL) | 112.0 ± 12.3 | 133.6 ± 17.5 | 0.011 |
| TG (mg/dL) | 94.1 ± 10.7 | 102.5 ± 9.8 | 0.049 |
| HDL-C (mg/dL) | 43.9 ± 8.92 | 30.9 ± 10.8 | 0.022 |
| VLDL-C (mg/dL) | 20.4 ± 7.94 | 24.5 ± 9.32 | 0.253 |
| LDL-C (mg/dL) | 59.2 ± 18.5 | 64.3 ± 30.8 | 0.052 |
| Zinc (µg/dL) | 115.4 ± 8.55 | 90.5 ± 10.0 | 0.01 |
| Midkine (ng/mL) | 149.6 ± 51.0 | 202.1 ± 47.4 | 0.003 |
Significance: A p-value of ≤ .05 was considered significant, Data represented as Mean ± SD, SD: Stander Deviation, n: Number of subjects, BMI: Body Mass Index, W/H: Waist to Hip Ratio, SBP: Systolic Blood Pressure, DBP: Diastolic Blood Pressure, TT3: Total Thyroxine, TT3: Total Triiodothyronine, TSH: Thyroid-Stimulating Hormone, FSG: Fasting Serum Glucose, HOMA-IR: Homeostatic Model Assessment for Insulin Resistance, QUICKI: Quantitative Insulin Sensitivity Check Index, T-CHO: Total Cholesterol, TG: Triglyceride, HDL-C: High Density Lipoprotein-Cholesterol, LDL-C: Low Density Lipoprotein-Cholesterol, VLDL-C: Very Low Density Lipoprotein-Cholesterol.
Table 1: Demographic and clinical characteristics for thyroid cancer patients and control groups.
The linear regression analysis shown in Table 2, the correlation between Serum Midkine and other biochemical studied in patients with thyroid cancer. No significant correlation was noticed between MDK and either biochemical parameters studied, except BMI, TSH, insulin and HOMA-IR have a significant positive correlation with Midkine level shown in Figure 1.
| Parameters | Midkine (ng/mL) | |
|---|---|---|
| Age (year) | r | -0.110 |
| P-value | 0.56 | |
| BMI (kg/m2) | r | 0.001 |
| P-value | 0.99 | |
| W/H | r | 0.078 |
| P-value | 0.68 | |
| TT3 (ng/mL) | r | 0.072 |
| P-value | 0.70 | |
| TT4 (ng/mL) | r | 0.123 |
| P-value | 0.51 | |
| TSH (µIU/mL) | r | 0.004 |
| P-value | 0.984 | |
| FSG (mg/dL) | r | 0.239 |
| P-value | 0.36 | |
| Insulin (µU/mL) | r | 0.028 |
| P-value | 0.88 | |
| HOMA-IR | r | 0. 05 |
| P-value | 0.050 | |
| QUICKI | r | -0.127 |
| P-value | 0.50 | |
| TC (mg/dL) | r | 0.113 |
| P-value | 0.55 | |
| TG (mg/dL) | r | 0.207 |
| P-value | 0.47 | |
| HDL-C (mg/dL) | r | -0.072 |
| P-value | 0.70 | |
| VLDL-C (mg/dL) | r | 0.090 |
| P-value | 0.63 | |
| LDL-C(mg/dL) | r | 0.129 |
| P-value | 0.49 | |
| Zinc (µg/dL) | r | -0.162 |
| P-value | 0.39 | |
Significance: P-value of ≤ .05 was considered significant, r: Person’s correlation, BMI: Body Mass Index, W/H: Waist to Hip Ratio, TT3: Total Thyroxine, TT3: Total Triiodothyronine, TSH: Thyroid-Stimulating Hormone. FSG: Fasting Serum Glucose, HOMA-IR: Homeostatic Model Assessment for Insulin Resistance, QUICKI: Quantitative Insulin Sensitivity Check Index, TC: Total Cholesterol, TG: Triglyceride, HDL-C: High-Density Lipoprotein-Cholesterol, LDL-C: Low-Density Lipoprotein Cholesterol, VLDL.C: Very Low Density Lipoprotein-Cholesterol.
Table 2: Correlation between levels of serum midkine and others biochemi cal studied in thyroid cancer patients group.
Discussion
The present study showed increased level of the novel adipocytokines (Midkine) in thyroid cancer group. Diagnosis of thyroid cancer has been facilitated by popularization of high-resolution US and whenever thyroid nodules are discovered clinically or incidentally, exclusion of malignancy gains importance [27]. However, its predictive value is still limited. Because it is invasive, the detection of malignancy depends in part on operator experience and may vary with respect to technical performance, non-diagnostic cytology rate is high, and also malignancy cannot be excluded in about 25% of thyroid nodules, possibly leading to unnecessary thyroid surgery [28]. Due to this limitation, researches have focused on genetic and markers that may aid in diagnosis and follow up [29].
The ratio of patients with increased Serum MK levels to total cancer patients examined agreed with that of patients with increased MK expression in tumor tissues reported previously [30,31]. Thus, MK expressed in carcinomatous tissues is probably secreted into the bloodstream, leading to an increase in serum MK level in cancer patients. It is notable that the increased expression of MK in carcinomatous tissues and the elevated serum MK levels in cancer patients did not show specification for a particular tissue. This is reminiscent of the case of p53 mutations in human carcinomas, suggesting the biological importance of MK in carcinogenesis. The role of MK in carcinogenesis and/ or tumor progression, as indicated by its transforming activities is consistent with this assumption [32,33]. Midkine is a heparin-binding growth factor that plays roles in growth, survival, inflammation/immunity, blood pressure, cellular proliferation, migration of cellular functions, angiogenesis, fibrinolysis, host defense and tissue protection, neurogenesis, and .It may enhance tumor invasion and therefore influence rates of survival [34].
The results of present study are close to those reported and the study involved three independent cohorts with a total of 933 participants including 388 HCC cases and 545 different controls enrolled from different medical centers [35]. Results showed that MDK levels were significantly elevated in HCC tissues as well as serum samples; serum MDK at the cutoff value of 0.654 ng/mL for HCC diagnosis showed an obviously higher sensitivity compared with AFP (86.9% versus 51.9%) with similar specificities (83.9% versus 86.3%); even in very early-stage HCC, the sensitivity of MDK was significant higher than AFP (80% versus 40%); in those AFP-negative HCC cases, the sensitivity could reach as high as 89.2%; and serum MDK level was significantly decreased in HCC patients after curative resection and elevated when tumor relapsed.
Midkine is frequently up-regulated in many types of cancer, including gastrointestinal, pancreatic, breast, and lung cancers, and melanoma [36]. MDK has been shown to have anti-apoptotic activity to embryonic and to Wilms’ tumor cells also promotes migration of various cells such as embryonic neurons neutrophils and macrophages [37]. These two activities of MK might be helpful in survival and invasion of tumor cells.
The results of present study were in agree with those of Kuzu, who found that both Serum Midkine (SMK) and Nodular Midkine (NMK) levels were higher in malignancy/suspicious nodules compared with benign nodules. They found that SMDK and NMDK levels were higher among patients with suspicious ultrasound features for malignancy [38].
According to another study, there was a significant difference in MDK levels, with thyroid nodule contour being higher in thyroid nodules with irregular contour than thyroid nodules with regular contour (P=0.001) and calcification being higher in microcalcification than macrocalcification (P=0.006) [39]. Between papillary cancer and follicular carcinoma, there was a statistically significant difference in MK levels (P=0.001).
Similarly, the Serum Midkine levels were considerably higher in patients with nodules that showed the following sonographic characteristics: In addition, Serum Medikine levels in suspicious/malignant nodules were substantially greater than in benign nodules (P 0.001) [40].
Infiltrating macrophages were the predominant source of Midkine in the neointima of atherosclerotic arteries, and those Midkine directly stimulates smooth muscle cell migration from the media to the intima, using an in-stent restenosis model of hypercholesterolemic rabbits. This highlights the functional link between Midkine knockdown and reduced inflammatory cell recruitment, particularly of innate immune cells. In the process of (neo) angiogenesis, monocytes are known to operate as permissive cells with the formation of collateral arteries and capillary sprouting. When monocytes are activated, they emit angiogenic cytokines and growth factors, such as MCP-1, TNF-, bFGF, and MMPs, to mention a few [41].
Conclusion
The current investigation found that thyroid cancer patients have considerably higher levels of Midkine than the control group. These results suggest that Midkine levels in thyroid cancer patients may be as a predictor marker against thyroid cancer complications. Further studies with larger population are needed to justify its performance in clinical search.
Acknowledgment
The authors thank the patients for their cooperation and the medical staffs in the laboratories of the “Diwaniya Teaching Hospital” in Al Qadisiyah
Conflict of Interest
The authors declare that they have no conflict of interest.
Funding
None.
References
- Davies, Louise, Luc GT Morris, Megan Haymart and Amy Y. Chen, et al. "American Association of Clinical Endocrinologists and American College of Endocrinology Disease State Clinical Review: The Increasing Incidence of Thyroid Cancer." Endocr Pract21 (2015): 686-696.
- Jung, Kyu-Won, Young-Joo Won, Chang-Mo Oh and Hyun-Joo Kong, et al. "Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2014." Cancer Res Treat 49 (2017): 292.
- Enewold, Lindsey, Kangmin Zhu, Elaine Ron and Aizen J. Marrogi, et al. "Rising Thyroid Cancer Incidence in the United States by Demographic and Tumor Characteristics, 1980-2005." Cancer Epidemiol Biomarkers Prev 18 (2009): 784-791.
- Dom, Geneviève, Maxime Tarabichi, K. Unger and G. Thomas, et al. "A Gene Expression Signature Distinguishes Normal Tissues of Sporadic and Radiation-Induced Papillary Thyroid Carcinomas." Br J Cancer 107 (2012): 994-1000.
- Meinhold, Cari L., Elaine Ron, Sara J. Schonfeld and Bruce H. Alexander, et al. "Nonradiation Risk Factors for Thyroid Cancer in the US Radiologic Technologists Study." Am J Epidemiol 171 (2010): 242-252.
- Borena, Wegene, Tanja Stocks, Håkan Jonsson and Susanne Strohmaier, et al. "Serum Triglycerides and Cancer Risk in the Metabolic Syndrome and Cancer (Me-Can) Collaborative Study." Cancer Causes Control 22 (2011): 291-299.
- Zhao, Z. G., X. G. Guo, C. X. Ba and W. Wang, et al. "Overweight, Obesity and Thyroid Cancer Risk: A Meta-Analysis of Cohort Studies." J Int Med Res 40 (2012): 2041-2050.
- Rezzónico, Jorge N, Mariana Rezzónico, Eduardo Pusiol and Fabian Pitoia, et al. “Increased Prevalence of Insulin Resistance in Patients with Differentiated Thyroid Carcinoma.” Metab Syndr Relat Disord 7 (2009):375-380.
- Biondi, Bernadette, Debora Arpaia, Paolo Montuori and Giuseppe Ciancia, et al. "Under the shadow of vesuvius: a risk for thyroid cancer?." Thyroid 22 (2012): 1296-1297.
- Pellegriti, Gabriella, Florent De Vathaire, Claudia Scollo and Marco Attard, et al. "Papillary Thyroid Cancer Incidence in the Volcanic Area of Sicily." J Natl Cancer Inst 101 (2009): 1575-1583.
- Jung, Su Kyoung, Kirang Kim, Kyung Tae and Gu Kong, et al. "The Effect of Raw Vegetable and Fruit Intake on Thyroid Cancer Risk among Women: A Case–Control Study in South Korea." Br J Nutr 109 (2013): 118-128.
- Cléro, Énora, Françoise Doyon, Vaïana Chungue and Frédérique Rachédi, et al. "Dietary Patterns, Goitrogenic Food, and Thyroid Cancer: A Case-Control Study in French Polynesia." Nutr Cancer 64 (2012): 929-936.
- Maan, Meenu, Jeffrey M. Peters, Mainak Dutta and Andrew D. Patterson. "Lipid Metabolism and Lipophagy in Cancer." Biochem Biophys Res Commun 504 (2018): 582-589.
- Bessesen, Daniel H. “Update on Obesity.” J Clin Endocrinol Metab 93 (2008): 2027-34.
- Zhang, Chi, Hua-Bing Wu, Meng-Xia Cheng, Ling Wang, Chao-Bing Gao, and Fen Huang. "Association of Exposure to Multiple Metals with Papillary Thyroid Cancer Risk in China." Environ Sci Pollut Res Int 26 (2019): 20560-20572.
- Petrosino, â?ªVincenzo, G. Motta, G. Tenore, M. Coletta, et al. "The Role of Heavy Metals and Polychlorinated Biphenyls (PCBs) in the Oncogenesis of Head and Neck Tumors and Thyroid Diseases: A Pilot Study." Biometals 31 (2018): 285-295.
- Garufi, Alessia, Valerio D'Orazi, Alessandra Crispini, and Gabriella D'Orazi. "Zn (II)-Curc Targets p53 in Thyroid Cancer Cells." Int J Oncol 47 (2015): 1241-1248.
- Ertek, Sibel, Arrigo FG Cicero, Omur Caglar, and Gurbuz Erdogan. "Relationship Between Serum Zinc Levels, Thyroid Hormones and Thyroid Volume Following Successful Iodine Supplementation." Hormones (Athens) 9 (2010): 263-268.
- Moncayo, Roy, Alexander Kroiss, Manfred Oberwinkler and Fatih Karakolcu, et al. "The Role of Selenium, Vitamin C, and Zinc in Benign Thyroid Diseases and of Selenium in Malignant Thyroid Diseases: Low Selenium Levels are Found in Subacute and Silent Thyroiditis and in Papillary and Follicular Carcinoma." BMC Endocr Disord 8 (2008): 1-12.
- Kadomatsu, Kenji, Mineko Tomomura, and Takashi Muramatsu. "cDNA Cloning and Sequencing of a New Gene Intensely Expressed in Early Differentiation Stages of Embryonal Carcinoma Cells and in Mid-Gestation Period of Mouse Embryogenesis." Biochem Biophys Res Commun 151 (1988): 1312-1318.
- Kato, Masako, Takao Shinozawa, Shinsuke Kato and Akira Awaya, et al. "Increased Midkine Expression in Hepatocellular Carcinoma: Immunohistochemical and In situ Hybridization Analyses." Arch Pathol Lab Med 124 (2000): 848-852.
- Muramatsu, Takashi. "Midkine and pleiotrophin: Two Related Proteins Involved in Development, Survival, Inflammation and Tumorigenesis." J Biochem 132 (2002): 359-371.
- Muramatsu, Takashi. "Midkine, A Heparin-Binding Cytokine with Multiple Roles in Development, Repair and Diseases." Proc Jpn Acad Ser B Phys Biol Sci 86 (2010): 410-425.
- Friedewald, William, R I Levy, and D S Fredrickson. “Estimation of the Concentration of Low-Density Lipoprotein Cholesterol in Plasma, without Use of the Preparative Ultracentrifuge.” Clin Chem 18 (1972): 499-502.
- Grzesiuk, WiesÅ?aw, Dorota Szydlarska, and Katarzyna Jóźwik. "Insulin Resistance in Endocrinopathies." Endocrinol Obes Metab Disorder 4 (2008): 38-44.
- Szurkowska, Magdalena, Krystyna Szafraniec, Aleksandra Gilis-Januszewska and Zbigniew SzybiÅ?ski, et al. "Insulin Resistance Indices in Population-Based Study and their Predictive Value in Defining Metabolic Syndrome." Przegl Epidemiol 59 (2005): 743-751.
- Cooper, David S, Gerard M Doherty, Bryan R Haugen, Richard T Kloos, et al. “Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer.” Thyroid 19 (2009): 1167-214.
- Jin, Judy and Christopher R. McHenry. "Thyroid Incidentaloma." Best Pract Res Clin Endocrinol Metab 26 (2012): 83-96.
- Patel, Hetal, Neerav Goyal and David Goldenberg. "Imaging, Genetic Testing, and Biomarker Assessment of Follicular Cell-Derived Thyroid Cancer." Ann Med 46 (2014): 409-416.
- Song, Xiao-Jun, Hisako Muramatsu, Kuniaki Aridome and Takashi Aikou, et al. "The Serum Level of Midkine, a Heparin-Binding Growth Factor, as a Tumor Marker." Biomed Res 18 (1997): 375-381.
- Ye, C, M. Qi, Q. W. Fan and K. Ito, et al. "Expression of Midkine in the Early Stage of Carcinogenesis in Human Colorectal Cancer." Br J Cancer 79 (1999): 179-184.
- Kadomatsu, Kenji, M. Hagihara, S. Akhter and Q. W. Fan, et al. "Midkine Induces the Transformation of NIH3T3 Cells." Br J Cancer 75 (1997): 354-359.
- Choudhuri, Rangana, Hua-Tang Zhang, Sandra Donnini and Marina Ziche, et al. "An Angiogenic Role for the Neurokines Midkine and Pleiotrophin in Tumorigenesis." Cancer Res 57 (1997): 1814-1819.
- Meng, Zhaowei, Jian Tan, Guizhi Zhang and Weijun Tian, et al. "Evaluation of Serum Midkine as a Biomarker in Differentiated Thyroid Cancer." Life Sci 130 (2015): 18-24.
- Zhu, Wen-Wei, Jia-Jian Guo, Lei Guo and Hu-Liang Jia, et al. "Evaluation of Midkine as a Diagnostic Serum Biomarker in Hepatocellular Carcinoma." Clin Cancer Res 19 (2013): 3944-3954.
- Muramatsu, Takashi. "Midkine, a Heparin-Binding Cytokine with Multiple Roles in Development, Repair and Diseases." Proc Jpn Acad Ser B Phys Biol Sci 86 (2010): 410-425.
- Horiba, Mitsuru, Kenji Kadomatsu, Eishin Nakamura and Hisako Muramatsu, et al. "Neointima Formation in a Restenosis Model is Suppressed in Midkine-Deficient Mice." J Clin Invest 105 (2000): 489-495.
- Kuzu, Fatih, Dilek Arpaci, Mustafa Unal and Ayfer Altas, et al. "Midkine: a novel biomarker to predict malignancy in patients with nodular thyroid disease." Int J Endocrinol 2016 (2016).
- Sheriba, Nermin Ahmed, Maram Mohamed Mahdy, Rana Hashem Ibrahim Elattary and Maha Mohamed El-Nabarawy. "Assessment of Serum Midkine Level in Benign and Malignant Thyroid Nodules. Can Midkine be a Marker of Thyroid Malignancy?." Thyroid Research and Practice 16 (2019): 95.
- Ibrahim, Nesma A., and Ahmed M. Hamam. "Role of Midkine in Predicting Malignancy in Patient with Solitary Thyroid Nodule." J Cancer Tumor Intl 9 (2019): 1-10.
- Qi, Maosong, Shinya Ikematsu, Nobuaki Maeda and Keiko Ichihara-Tanaka, et al. "Haptotactic Migration Induced by Midkine: Involvement of Protein-Tyrosine Phosphatase ζ, Mitogen-Activated Protein Kinase, and Phosphatidylinositol 3-Kinase." J Biol Chem 276 (2001): 15868-15875.
Citation: Gebur, Noor Ali and Hanaa Addai Ali. "Association between Levels of Serum Midkine with Insulin Resistance as New Potential Diagnostic Marker for Thyroid Cancer in its Early Stages." Clin Schizophr Relat Psychoses 15S(2021). Doi: 10.3371/ CSRP.GNAH.081221.
Copyright: © 2021 Gebur NA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.