Research Article - Clinical Schizophrenia & Related Psychoses ( 2021) Volume 0, Issue 0
2Department of Gynecology, Shahid Beheshti University of Medical Sciences, Tehran, Iran
3Department of Ophthalmology, Stanford University School of Medicine, Stanford, USA
Mohammad Nasiri, Department of Surgery, Rasool e Akram Hospital, Tehran, Iran, Email: moham.nasiri@gmail.com
Received: 16-Dec-2021 Accepted Date: Dec 30, 2021 ; Published: 06-Jan-2022
Abstract
Background and aim: The COVID-19 pandemic has negatively affected all sections of society, including medical staff. Based on a review study, the aim of this study was to look at the impact of the COVID-19 pandemic on surgical residents, educational process, surgical, and mental health components.
Material and methods: The results of this study were based on the method of review studies. To conduct this study, a systematic search of international databases including Web of Science, Science Direct, Scopus, PubMed, and Google Scholar between 2000 and 2021 was first performed using related keywords. Finally, 30 articles were chosen based on the scope and the necessary criteria for obtaining data, and the needed results were extracted from them.
Results: The results showed that 6776 residents and 220 program managers participated in these studies, with the largest sample sizes coming from the United States (3187 people), India (716 people) and Italy (661 people), respectively. Furthermore, the results showed that the COVID-19 pandemic had a negative effect on surgical residents', educational activities, as well as mental health, and surgical activities.
Conclusion: Based on the results, it can be concluded that COVID-19 pandemic has a negative effect on surgical residents' educational process, as well as increased their anxiety and stress, and for that reason, proper planning by managers is needed to reduce these negative effects.
Keywords
COVID-19 • Pandemic • Training • Operative • Mental health • Surgical residents
Introduction
Since December 2019, a global epidemic of the new coronavirus (COVID-19), also known as severe acute respiratory syndrome, has emerged, posing a threat to the health and lives of millions of people around the world [1]. Other acute respiratory disorders, such as Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS), have been identified by the World Health Organization (WHO) in the last two decades. The mortality rate due to SARS disease is recorded to be 8096 people in 29 countries, and the mortality rate due to MERS disease is reported to be 858 people in 27 countries [2]. However, the mortality rate from the COVID-19 disease is even higher, with more than 3.3 million individuals worldwide having died from this epidemic until May/11/2021. The greatest concern about COVID-19 comes from the fact that the disease's occurrence and mortality are increasing day after day, and the rate of medication differs throughout the world. Since not everyone in the world has access to vaccines, this epidemic will continue to cause anxiety and concern for a long time.
Going to declare a state of emergency, governments and public health systems have taken comprehensive steps to prevent the disease from spreading. Millions of people around the world have changed their lifestyles as a result of the disease [3]. Furthermore, the rate of disease transmission and the resulting mortality has caused considerable anxiety among people all over the world [4].
The physical and mental health of both ordinary citizens and medical staff has been influenced by the disease's stress and its adverse psychosocial impacts [5-9]. In their study, Al-Rabiaah, et al. found that medical professionals are not excluded from this rule or principle, and that they are often influenced by these psychological stresses. This medical staff group may also be much more vulnerable than other people in the community, and they also have higher rates of depression and anxiety [9- 11].
In medicine, dentistry, and veterinary medicine, surgery is one of the possible treatments or operations. Of course, the knowledge and techniques of this method are also called surgery. In this process, an incision is usually made to remove a part of the body (such as the gallbladder, tonsils, or appendix) or infectious or cancerous tissue, or to insert a tube or device (such as a prosthesis or prosthetic valve), or to manipulate, fix, and correct a defect (such as suturing an aneurysm or opening a vein) has been used [12].
Surgery is one of the most important medical professions that many people need, resulting in the development of various areas of surgery for the majority of the human body. The most significant and well-known areas related to surgery are general surgery, plastic surgery, heart surgery, vascular and trauma surgery, pediatric surgery, chest and cardiothoracic surgery, orthopedic surgery, obstetrics and gynecology surgery, kidney and urinary tract surgery, neurological surgery, Otorhinolaryngology and/or otolaryngology (ENT) surgery, rhinoplasty, eye (ocular) surgery, laryngeal surgery, periodontal (gum) surgery, oral and maxillofacial surgery are the most important and famous fields related to surgery. Considering that the most of a patient's organs may require surgery, and therefore this field of medicine can be considered as the most important, relevant and necessary field for patient treatment.
As previously stated, medical staff can suffer severe stress and anxiety as a result of the specific situations they encounter while faced with COVID-19 patients, and this may have an impact on their learning during training, working conditions, and mental health, as well as greatly impress surgeons and residents in this field [5-9]. However, up to date, only one review study has been conducted on the effect of COVID-19 pandemic on the educational activity of surgical residents [13], however, since the mentioned study consisted primarily on studies conducted in 2020 and focuses mainly on the effect of this pandemic on the educational process of surgical residents, and since the COVID-19 pandemic is still affecting most countries in 2021, the need for studies conducted in 2021 for the topic in question is also critical. In addition to the educational aspect, it is necessary to pay attention to other aspects of the COVID-19 pandemic effect, including burnout, operative activity, mental health, working conditions and quality, as well as the personal life of surgical residents, which will be addressed in this study as much as possible.
Because of the above reasons, the main purpose of this study is to investigate the impact of COVID-19 pandemic on working conditions, educational status and learning as well as the mental health status of surgeons and surgical residents by reviewing previous and similar studies.
Material and Methods
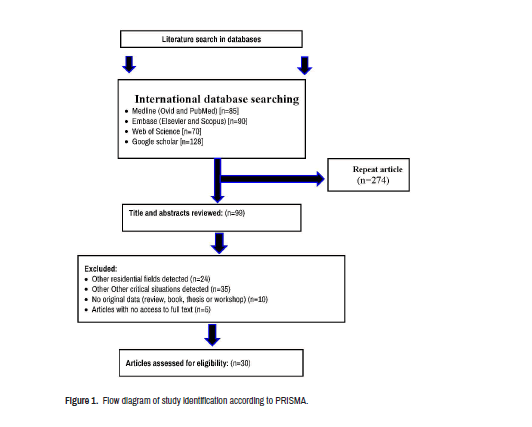
Systematically search globally accessible databases such as Web of Science, Science Direct, Scopus, PubMed, and Google Scholar from December 2000 to May 2021 in order to review and collect the required data from published articles and reviews relating to the topic under study. Systematic review using Mesh terms "COVID-19", "surgical", "surgeons", "psychological", "residents", "impact", "training", "pandemic", "work", "Medical", "Coronavirus 2019", "Coronavirus 2019", "Operative impact", "mental health", "stress", "anxiety", "educational", "hospital", "job Status", "working patterns", "operation", "effect", "Response", "time of COVID-19", "during of COVID-19", "Residents' Perspective", "training program", "general surgery", "Online education", "coping strategies", "learning" was done. The same Mesh terms were used in other databases in a similar way. To ensure that the search was systematic, the references of the studies that were found were checked (Reference Checking) to exclude the possibility of missing studies. Figure 1 was used to study citation tracing, and texts were checked and articles were received through using PRISMA guidelines [14]. Moreover, informal papers, articles published in the letter-to-the-editor format, as well as unpublished articles and content from websites were also removed from the list of files to be accessed. Finally, for this study, the results of 30 published articles were reviewed.
Results and Discussion
A total of 373 different types of articles and reports were initially listed for the current study based on the search strategy (Figure 1). Since there are several target groups for the topic under study, including various fields of medicine, and also for the subject under consideration, several studies were conducted prior to the COVID-19 pandemic, and as a result, the initial articles collected were many. Finally, 30 articles were chosen based on the inclusion criteria, and the required results were extracted from their full text and listed in Table 1.
| The most important outputs of the study | Specialized field | Subject under study | Number of participants/ programme directors | Study location | Study |
|---|---|---|---|---|---|
|
Cardiothoracic, General Surgery, Neurosurgery, Orthopedics, Otolaryngology/Head and Neck Surgery, Plastics, Urology, and Vascular Surgery |
Impact on education |
146 | USA |
Wise et al. [19] |
|
General surgery |
Impact on stress and psychological | 234 | Saudi Arabia and Bahrain |
Aljehani et al. [20] |
|
General surgery | Impact on operative volume | Not applicable | Chile |
Inzunza et al. [21] |
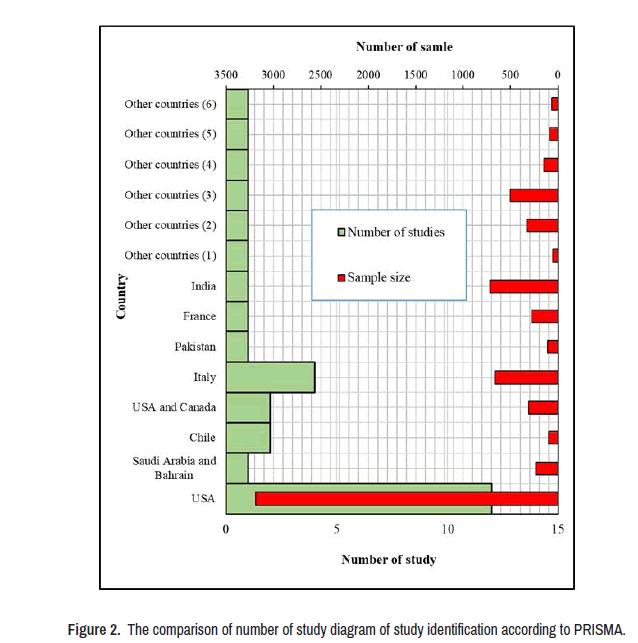
After reviewing the studies, it was discovered that the majority of them were linked to the United States (12 studies) and Italy (4 studies), with just 1-2 studies performed in the remaining countries. Based on the current results of the reviewed studies [15-18], 6776 residents and 220 program managers actively participated in these studies, with the highest sample sizes in the United States (3187 people), India (716 people), and Italy (661 people), respectively (Figure 2).
The results of the present study showed that the amount of Operative Activity (OA) has decreased in the majority of studies performed in various countries. For example, in the study of Inzunza et al. in Chile, the rate of OA reduction was reported to be 61.7%, while this reduction rate in the United States in the studies of Purdy et al. and Collins et al. were reported to be 33.5% and 63.3%, respectively. Other studies, including Givi et al., Zoia et al., Burks et al., Aziz et al., Paesano et al., Kapila et al., and Munjal et al., have identified other methods of reducing OA, however the precise sum of OA has not been reported, whereas, the higher incidence of surgical case cancellations[19-20], as well as the decline in the participation of surgical trainees in surgical centers and hospitals, have been specifically highlighted in these studies Surgical trainees have expressed concern about the reduction in the number of surgical cases and the lack of in- person teaching of the surgical process. This confusion comes mostly from a lack of practical surgical knowledge as well as experience doing prospective job duties [21-27].
Some studies have shown that during the COVID-19 pandemic, some surgical trainees engaged in non-surgical medical treatment rather than doing surgery, which is a negative influencing factor in terms of gaining experience and learning the fundamentals of surgery.
The results of the present study showed that most surgical residents in various studies felt that due to the COVID-19 pandemic, their educational activities were negatively affected. For example, in the studies of Alhaj et al., Zingaretti et al., Bernardi et al., Figueroa et al., Ferrara et al., Paesano et al. and Munjal et al. have clearly reported the negative impact of the COVID-19 pandemic on the surgical education process [28-36].
Due to the decrease in clinical and surgical operations conducted by trainees since the COVID-19 pandemic, so the duration of their theoretical training activities outside of surgical centers and hospitals has increased. Most studies have reported that the way of conducting training sessions has changed from face-to-face to virtual due to the reduction of face-to-face meetings to prevent the transmission of the coronavirus. However, some limited studies have shown that the virtual model of teaching surgery is less efficient and effective than the face-to-face method. This viewpoint indicates that keeping a virtual training process may have a negative impact on surgical trainees' ability to achieve experiences and create anxiety about their future careers [13]. In some articles, it has been reported that due to the decrease in the clinical activity of surgical trainees, they have more opportunities to conduct research activities as well as the use of updated and new scientific articles and reports, which is clearly stated in the study of Zoia et al. [25].
One of the other effects of the COVID-19 pandemic, in addition to impacting educational, clinical, and surgical activities, was the psychological impact of the crisis on surgical trainees, which has been clearly reported in several previous studies. Numerous surgical trainees suffer anxiety and stress as a result of exposure to the COVID-19 pandemic, according to studies by An et al., Alhaj et al., Abdessater et al., Bar et al., Collins et al., Kapila et al., Mishra et al. and Khusid et al. Furthermore, it has been stated in these studies that some surgical trainees are concerned about transmitting the coronavirus to their families and loved ones when they are exposed to patients with COVID-19 [37-48].
Given that the COVID-19 pandemic has decreased surgical residents' operative volume, this has reduced burnout in them, as noted and confirmed in the study by Abdelsattar et al. [22], while Aziz et al. reported that 33.1% of general surgery residents' burnout during the COVID-19 pandemic was higher than during the pre-pandemic period [38].
Conclusion
Based on the results of the present study, it can be concluded that the COVID-19 pandemic has had significant effects on educational process, surgical activities, mental health and burnout of surgical trainees around the world. In most parts of the world, due to the fear of COVID-19, the operative volume has decreased and unfortunately this has had a negative impact on the training and learning process of trainees because trainees share a large part of their experiences in person while watching and participating in a surgical operation and they will then get actual surgery, which was canceled during the COVID-19 pandemic. In terms of educational dimension, most trainees feel that the pandemic has had a negative impact on their educational experiences, and in terms of mental health, most surgical trainees have encountered stress and anxiety as a result of the pandemic. Reduced burnout and further opportunities for research activities are among the positives of this pandemic for surgical trainees. Most various studies around the world have reported that most of the educational activities of surgical residents are performed by virtual methods. Finally, based on the results of the present review study, it can be concluded that the COVID-19 pandemic has a great negative impact on educational activities, surgical activities as well as mental health of surgical residents and that the necessary conditions, facilities and strategies to prevent the negative effects of this pandemic to all clinical personnel, including surgical residents, should be provided by the relevant officials and managers of the treatment department.
References
- Darvishi, Mohammad, Hamze Shahali and Azade Amirabadi Farahani. “Guillain-Barré Syndrome Associated with SARS-CoV-2 Infection: A Case Report.” Eur J Transl Myol 31 (2021).
- Huang, Junjie, Jeremy Yuen-Chun Teoh, Sunny H Wong and Martin Wong. “The Potential Impact of Previous Exposure to SARS or MERS on Control of the COVID-19 Pandemic.” Eur J Epidemiol 35 (2020): 1099-1103.
- Di Renzo, Laura, Paola Gualtieri, Francesca Pivari and Laura Soldati, et al. “Eating Habits and Lifestyle Changes During COVID-19 Lockdown: An Italian Survey." J Transl Med 18 (2020): 1-15.
- Mirzaee, Seyed Mohammad Mousavi, Fabrício Guimarães Gonçalves, Mahyar Mohammadifard and Shirin Mojgan Tavakoli, et al. “Focal Cerebral Arteriopathy in a Pediatric Patient with COVID-19.” Radiology 297 (2020): e274-e275.
- Ning, Xianjun, Fang Yu, Qin Huang and Xi Li et al. “The Mental Health of Neurological Doctors and Nurses in Hunan Province, China During the initial stages of the COVID-19 Outbreak.” BMC Psychiatry 20 (2020): 1-9.
- Khan, Zahid Hussain, Shahram Samadi, Jalil Makarem, and Seyed Mohamad Mireskandari. “Tests with Proven Value in Diagnosis of COVID-19.” Iran J Microbiol 12 (2020): 261.
- Guillain-Barré Syndrome Associated with SARS-CoV-2 Infection: A Case Report
- Mousavi-Hasanzadeh, M, Kamali, A Safi and F Sarmadian, et al. “Clinical Characteristics and Short-term outcomes of Patients with severe COVID-19.” Indian J Forensic Med Toxicology 15 (2021):2691–2694.
- Al-Rabiaah, Abdulkarim, Mohamad-Hani Temsah, Ayman A Al-Eyadhy and Gamal M Hasan, et al. “Middle East Respiratory Syndrome-Corona Virus (MERS-CoV) Associated Stress among Medical Students at a University Teaching Hospital in Saudi Arabia.” J Infect Public Health 13 (2020): 687-691.
- Xiang, Yu-Tao, Yuan Yang, Wen Li and Ling Zhang, et al. “Timely Mental Health Care for the 2019 Novel Coronavirus outbreak is Urgently Needed.” Lancet Psychiatry 7 (2020): 228-229.
- Li, Wen, Yuan Yang, Zi-Han Liu and Yan-Jie Zhao, et al. “Progression of Mental Health Services during the COVID-19 outbreak in China.” Int J Bio Sci 16 (2020): 1732.
- F. Charles Brunicardi, Dana K. Andersen, Timothy R. Billiar and David L. Dunn, et al. Schwartz's Principles of Surgery. New York: McGraw-Hill Education, USA, (2004).
- Hope, C, JJ Reilly, G Griffiths and J Lund, et al. “The Impact of COVID-19 on Surgical Training: A Systematic Review.” Tech Coloproctol 25 (2021): 505-520.
- Aljehani, Yasser M, Sharifah A Othman, Nosibah K Telmesani and Raghad A Alghamdi, et al. “Stress and Psychological Resilience among General Surgery Residents during COVID-19 Pandemic.” Saudi Med J 41 (2020): 1344.
- Inzunza, MN, Besser and F Bellolio. “Decrease in Operative Volume in General Surgery Residents in Chile: Effects of the COVID-19 Pandemic.” Br J Surg 108 (2021): e226-e227.
- Wady H, Restle D Park J and Pryor A et al. “The Role of Surgeons During the COVID-19 Pandemic: Impact on Training and Lessons Learned from a Surgical Resident’s Perspective.” Surg Endosc 14 (2020):1-7.
- Wise, Clare Elizabeth, Sylvia Bereknyei Merrell, Marzena Sasnal and Joseph D Forrester, et al. “COVID-19 Impact on Surgical Resident Education and Coping.” J Surg Res 264 (2021): 534-543.
- Moher D, Liberati A, Tetzlaff J and Altman DG. “Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement.” Int J Surg 5 (2010): 336-41.
- Wise, Clare Elizabeth, Sylvia Bereknyei Merrell, Marzena Sasnal and Joseph D Forrester, et al. “COVID-19 Impact on Surgical Resident Education and Coping.” J Surg Res 264 (2021): 534-543.
- Aljehani, Yasser M, Sharifah A Othman, Nosibah K Telmesani and Raghad A Alghamdi, et al. “Stress and Psychological Resilience among General Surgery Residents During COVID-19 Pandemic.” Saudi Med J 41 (2020): 1344.
- Inzunza M, Besser N, Bellolio F. “Decrease in Operative Volume in General Surgery Residents in Chile: Effects of the COVID-19 Pandemic.” Br J Surg 22 (2021):24.
- Abdelsattar, Jad M, Julia R Coleman, Alisa Nagler and Mohsen Shabahang, et al. “Lived Experiences of Surgical Residents During the COVID-19 Pandemic: A Qualitative Assessment.” J Surg Educ 78 (2021): 1851-1862.
- Purdy, Amanda C, Christian De Virgilio, Amy H Kaji and Edgar Shields Frey, et al. “Factors Associated with General Surgery Residents’ Operative Experience during the COVID-19 Pandemic.” JAMA Surg 156 (2021): 767-774.
- Givi, Babak, Michael G Moore, Arnaud F Bewley and Charles S Coffey, et al. “Advanced Head and Neck Surgery Training during the Covid‐19 Pandemic.” Head Neck 42 (2020): 1411-1417.
- Zoia, Cesare, Giovanni Raffa, Teresa Somma and Giuseppe M Della Pepa, et al. "COVID-19 and Neurosurgical Training and Education: An Italian Perspective.” Acta Neurochir 162 (2020): 1789-1794.
- An, Tonya W, Jensen K Henry, Oduche Igboechi and Pengcheng Wang, et al. “How are Orthopaedic Surgery Residencies Responding to the COVID-19 Pandemic? An Assessment of Resident Experiences in Cities of Major Virus Outbreak.” J Am Acad Orthop Surg 28 (2020):79-85.
- White, Erin M, Matthew P Shaughnessy, Andrew C Esposito and Martin D Slade, et al. “Surgical Education in the Time of Covid 19: Understanding the Early Response of Surgical Training Programs to the Novel Coronavirus Pandemic." J Surg Educ 78 (2021): 412-421.
- Alhaj, Ahmad K, Tariq Al-Saadi, Fadil Mohammad and Said Alabri. “Neurosurgery Residents' Perspective on COVID-19: Knowledge, Readiness, and Impact of this Pandemic.” World Neurosurg 139 (2020): e848-e858.
- Zingaretti, Nicola, Filippo Contessi Negrini, Alessandro Tel and Marco Mario Tresoldi, et al. “The Impact of COVID-19 on Plastic Surgery Residency Training.” Aesthetic Plast Surg 44 (2020): 1381-1385.
- Bernardi, Laura, Paola Germani, Giulio Del Zotto, Giovanni Scotton and Nicolò de Manzini. “Impact of COVID-19 Pandemic on General Surgery Training Program: An Italian Experience.” Am J Surg 220 (2020): 1361-1363.
- Megaloikonomos, Panayiotis D, Martin Thaler, Vasilios G Igoumenou and Tommaso Bonanzinga, et al. “Impact of the COVID-19 Pandemic on Orthopaedic and Trauma Surgery Training in Europe.” Int Orthop 44 (2020): 1611-1619.
- Osama, Muhammad, Farhan Zaheer, Hasham Saeed and Khadija Anees, et al. “Impact of COVID-19 on Surgical Residency Programs in Pakistan; a Residents' Perspective. Do Programs Need Formal Restructuring to Adjust with the “New Normal”? A Cross-Sectional Survey Study.” Int J Surg 79 (2020): 252-256.
- Figueroa, Francisco, David Figueroa, Rafael Calvo-Mena and Felipe Narvaez, et al. “Orthopedic Surgery Residents’Perception of Online Education in their Programs during the COVID-19 Pandemic: Should it be Maintained after the Crisis?” Acta Orthopaedica 91 (2020): 543-546.
- Abdessater, Maher, Morgan Rouprêt, Vincent Misrai and Xavier Matillon, et al. “COVID-19 Pandemic Impacts on Anxiety of French Urologist in Training: Outcomes from a National Survey.” Prog Urol 30 (2020): 448-455.
- Amparore, Daniele, Francesco Claps, Giovanni E Cacciamani and Francesco Esperto, et al. “Impact of the COVID-19 Pandemic on Urology Residency Training in Italy.” Minerva Urol Nefrol 72 (2020): 505-509.
- Brar, Branden, Mohamed Bayoumy, Andrew Salama and Andrew Henry, et al. “A Survey Assessing the Early Effects of COVID-19 Pandemic on Oral and Maxillofacial Surgery Training Programs.” Oral Surg Oral Med Oral Pathol Oral Radiol 131 (2021): 27-42.
- Burks, Joshua D, Evan M Luther, Vaidya Govindarajan and Ashish H Shah, et al. “Early Changes to Neurosurgery Resident Training during the COVID-19 Pandemic at a Large US Academic Medical Center.” World Neurosurg 144 (2020): e926-e933.
- Aziz, Hassan, Tayler James, Daphne Remull and Linda Sher, w et al. “Effect of COVID-19 on Surgical Training Across the United States: A National Survey of General Surgery Residents.” J Surg Educ 78 (2021): 431-439.
- Collins, Caitlin, Kelly Mahuron, Tasce Bongiovanni and Elizabeth Lancaster, et al. “Stress and the Surgical Resident in the COVID-19 Pandemic.” J Surg Educ 78 (2021): 422-430.
- Ferrara, Mariantonia, Vito Romano, David H Steel and Rajen Gupta, et al. “Reshaping Ophthalmology Training after COVID-19 Pandemic.” Eye 34 (2020): 2089-2097.
- Paesano, Nahuel, Fernando Santomil and Ignacio Tobia. “Impact of COVID-19 Pandemic on Ibero-American Urology Residents: Perspective of American Confederation of Urology (CAU).” Int Braz J Uro 46 (2020): 165-169.
- Kapila, AK, Y Farid, V Kapila and M Schettino, et al. “The Perspective of Surgical Residents on Current and Future Training in Light of the COVID-19 Pandemic.” Br J Surg 107 (2020): e305-e305.
- Mishra, Deepak, Akshay Gopinathan Nair, Rashmin Anilkumar Gandhi and Parikshit J Gogate, et al. “The Impact of COVID-19 Related Lockdown on Ophthalmology Training Programs in India–Outcomes of a Survey.” Indian J Ophthalmol 68 (2020): 999.
- Khusid, Johnathan A, Corey S Weinstein, Adan Z Becerra and Mahyar Kashani, et al. “Well‐being and Education of Urology Residents during the Covid‐19 Pandemic: Results of an American National Survey.” Int J Clin Pract 74 (2020): e13559.
- Munjal, Tina, Katherine R Kavanagh, Rami M Ezzibdeh and Tulio A Valdez. “The Impact of COVID-19 on Global Disparities in Surgical Training in Paediatric Otolaryngology.”Int J Pediatr Otorhinolaryngol 138 (2020): 110267.
- Pelargos, Panayiotis E, Arpan Chakraborty, Yan D Zhao, Zachary A Smith and Ian F Dunn, et al. “An Evaluation of Neurosurgical Resident Education and Sentiment during the Coronavirus Disease 2019 Pandemic: A North American Survey.” World Neurosurg 140 (2020): e381-e386.
- Rosen, Geoffrey H, Katie S Murray, Kirsten L Greene and Raj S Pruthi, et al. “Effect of COVID-19 on Urology Residency Training: A Nationwide Survey of Program Directors by the Society of Academic Urologists.” J Urol 204 (2020): 1039-1045.
- Zheng, Jian, Mautin Hundeyin, Katherine He and Teviah Sachs, et al. “General Surgery Chief Residents’ Perspective on Surgical Education during the Coronavirus Disease 2019 (COVID-19) Pandemic.” Surgery 168 (2020): 222-225.
Citation: Alireza Negahi, Nahid Nafissi, Foolad Eghbali, and Behnaz Nouri, et al. “A Literature Review about Impact of COVID-19 on Operative Activity, Educational Process and Mental Health of Surgical Residents” Clin Schizophr Relat Psychoses 15S(2021).Doi: 10.3371/CSRP.NANN.010622.
Copyright: © 2021 Negahi A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.